Family Centered Cesarean with See Baby
I love it when the mom writes the blog post for me 🙂 It’s her birth, so I feel it should be her story to tell, from her own perspective.
This birth story took place at Dekalb Medical with See Baby
“It was Thursday April 6th and I was 41 weeks and 1 day. We went for my routine weekly office visit around 1:00 p.m. After checking my vitals a few times the midwife informed me that my BP reading was an object of concern because it was elevated into the realm of stroke level. The nurse wouldn’t tell me what the first four readings were in an effort to not upset me too much, but I did manage to find out the last one (one of the lowest) was 189/100. This was definitely high enough for concern; especially because throughout my pregnancy BP had never been an issue. They told us they wanted to send us over to the hospital to get some tests done and make sure everything else in my body was still functioning properly. Luckily Corey, being the over planner he is had already packed our bags in the car so we headed to the hospital and checked in around 4:30 p.m.
The plan once we saw the midwife on call was to get my BP down, take some blood to check my liver (or maybe it was kidney, I forgot) and then hopefully send me home to let our birthing time start naturally whenever it was meant to. Because we were past 41 weeks they decided to do an ultrasound just to check on baby since we were there and make sure everything was ok.

After giving me some medicine via IV for my BP the ultrasound tech came in and when looking kindly told us we wouldn’t be going home that night because my amniotic fluid level was pretty low. Once we found that out the midwife returned and told us she had spoken to Dr. Bootstaylor who had said there was no reason in chasing my blood pressure just to get that down, especially with the amniotic fluid level being low, so induction was recommended.
We got checked into a room and had some dinner (Corey went and got bbq as a last supper before the big event kind of deal) and about 9:30 that evening they gave me a dose of cervidil to help ripen my cervix. I was only dilated at a 1 and the plan was for the medicine to speed up that process so we could hopefully still have our natural water birth as planned. About 20 mins after they inserted the medicine the pressure waves started pretty strong. After a while it became apparent that they were going to stay strong and consistent for the entire 12 hour duration of the medicine being in. The nurses were very respectful of our wishes and pretty much left us undisturbed the majority of the night. Unfortunately because of my blood pressure, baby and I both were required to be hooked up to continuous monitoring, meaning I couldn’t leave the bed for more than a few minutes at a time.
The consistent strong pressure waves (one of the effects for some women of cervidil is start of birthing time, but sadly for me there was no natural progression, it all just sort of slammed started at high intensity real quick) and the restricted movement kept me (and in turn Corey) up the entire night and by the time they returned to remove the medicine at 9:30 a.m. I was an exhausted mess. After they took out the cervidil I was 4 cm dilated and my body was naturally having pressure waves every 1-2 mins, so they ruled out using pitocin and said another round of cervidil was necessary to continue the dilation process. Our biggest concern at that point was another 12 hours would literally leave me drained to the point of exhaustion by the time we got to the actual delivery time.
After we consulted with Maegan about our options we ended up opting for an epidural so that I could at least attempt to rest and ideally get some energy back before the real show started.

About 5 mins after the epidural I was able to sleep for only about 10 minutes before the midwife returned to let us know that they’d noticed the baby’s heart rate dropping with each pressure wave prior to the epidural and there were hopes that it might stop after I got it, but it was continuing to drop with every wave indicating the baby was in distress.
After talking to Dr. B, much against what he wanted to recommend, his recommendation at that point because of baby’s condition was a family centered c-section.
We asked for some time and talked to Maegan again so we could be sure we were asking the right questions we wanted to know.
After asking if waiting an hour or two was an option (to see if I would fully dilate) we were told that we could definitely choose to do that, but on a scale of 1,2,3 (1 being the least, 3 the highest) where they measure baby’s heart rate dropping he was already at a 3.
With each drop over time the pH in his blood level would change and could lead to brain damage. At that point we tossed our other questions knowing that his safety was our priority and after talking with the midwife and OB knew that they were coming from view of doing what was best for baby and we trusted them fully.

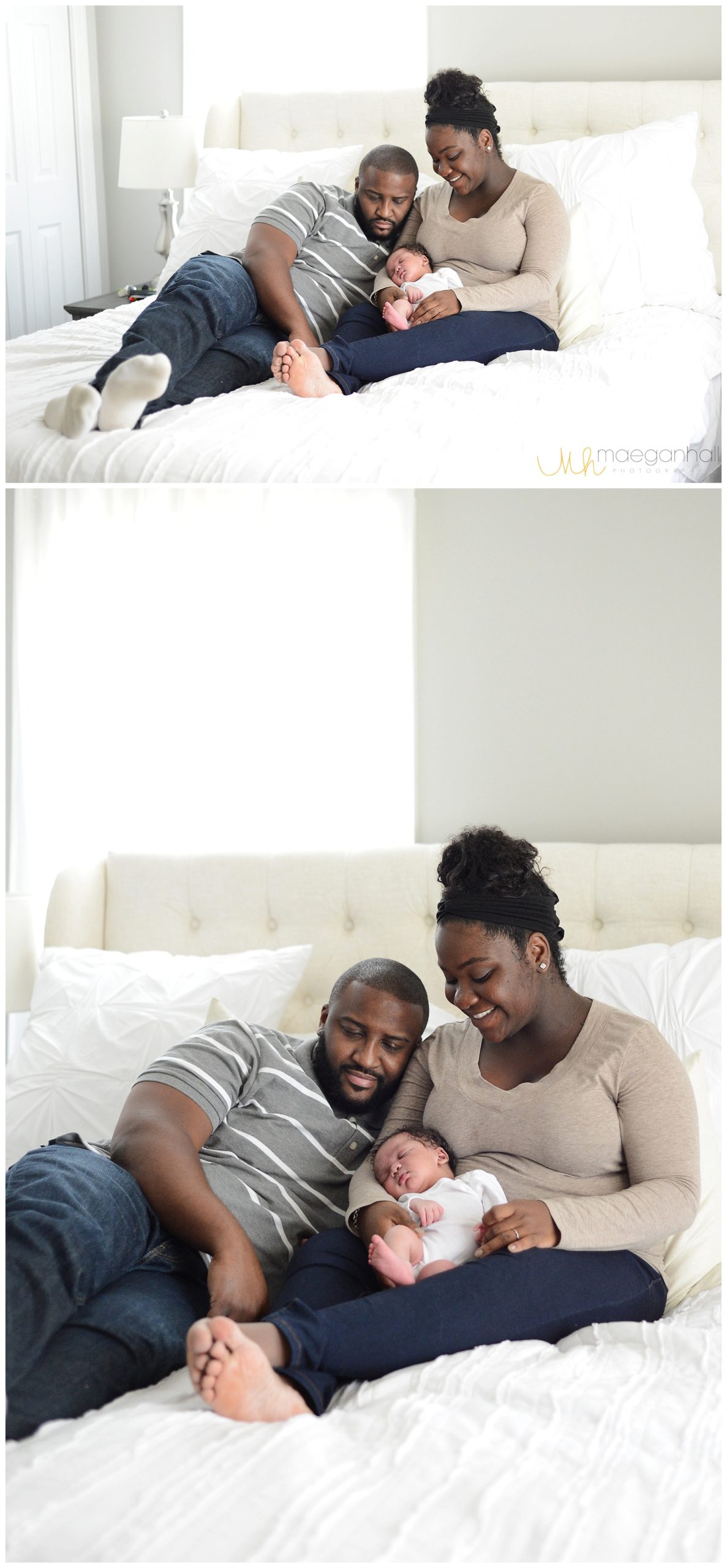
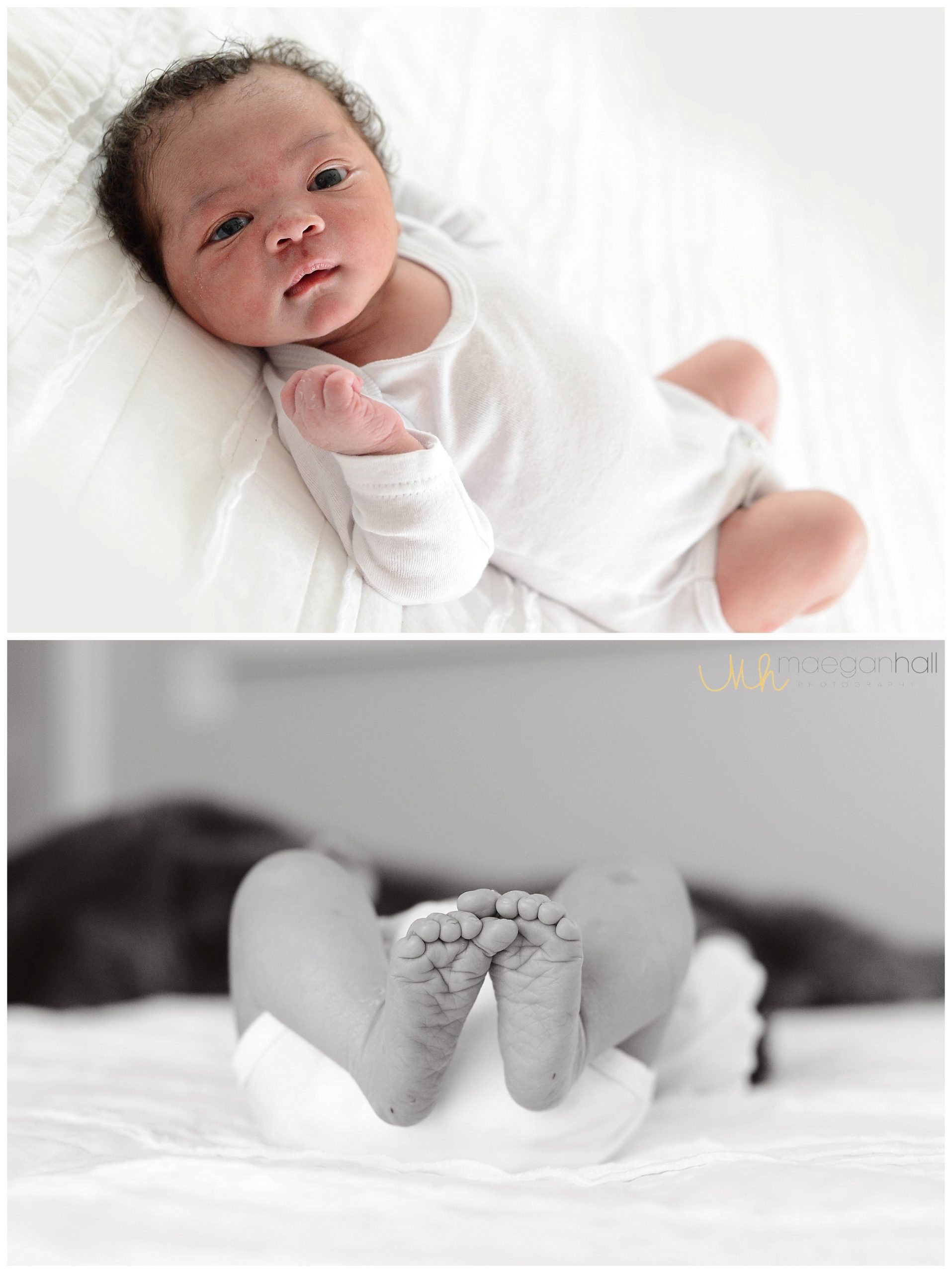
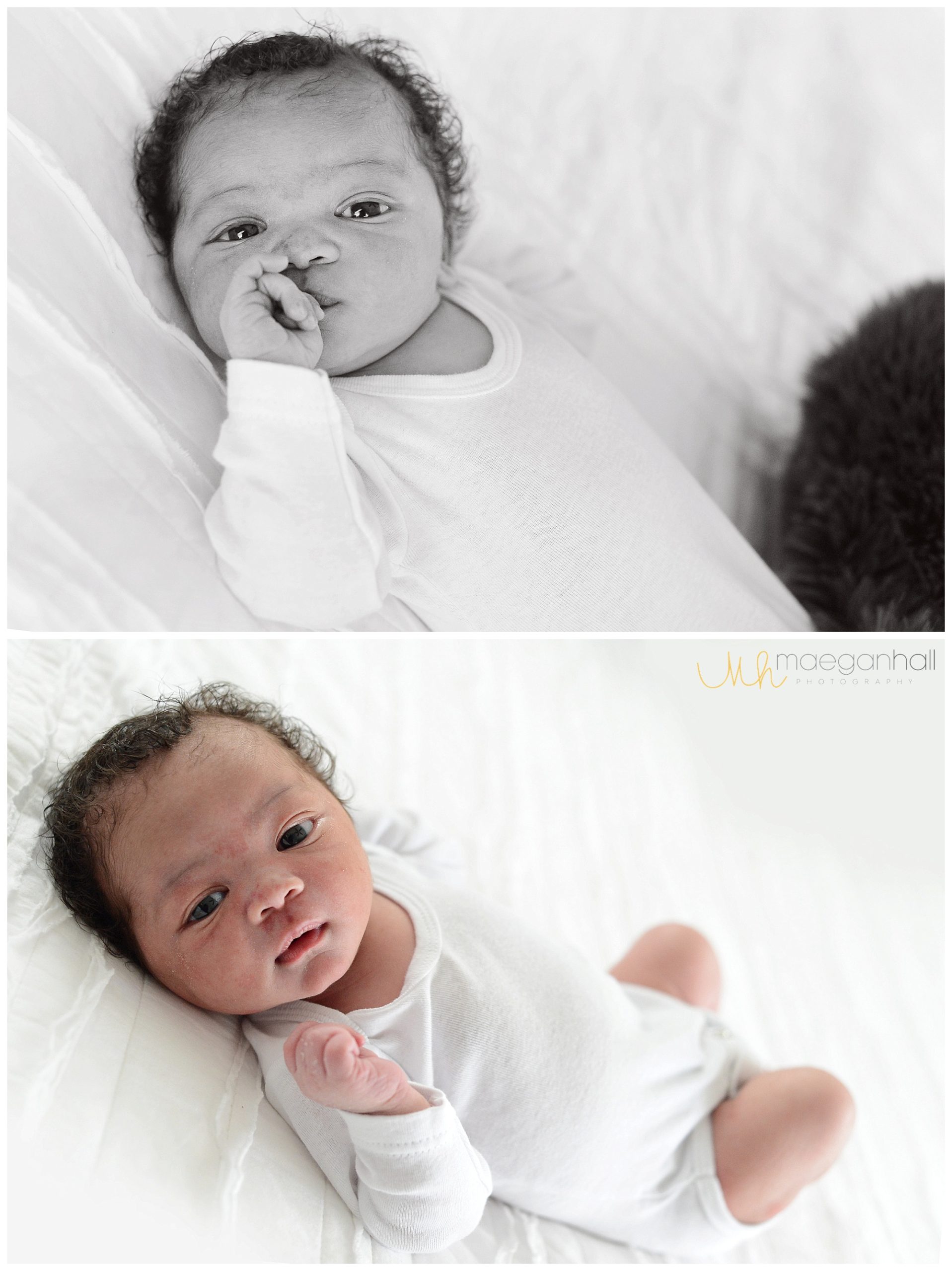
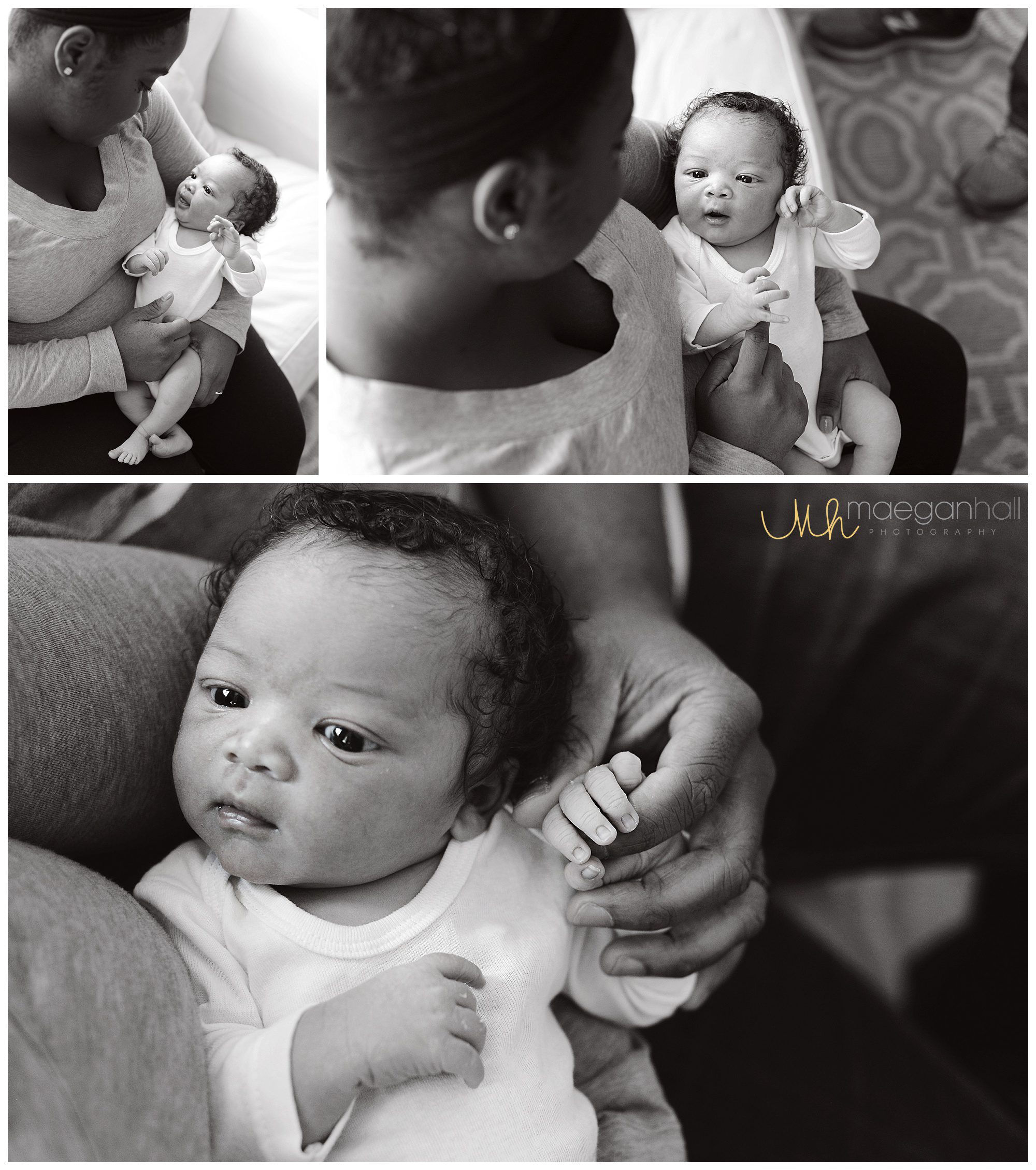
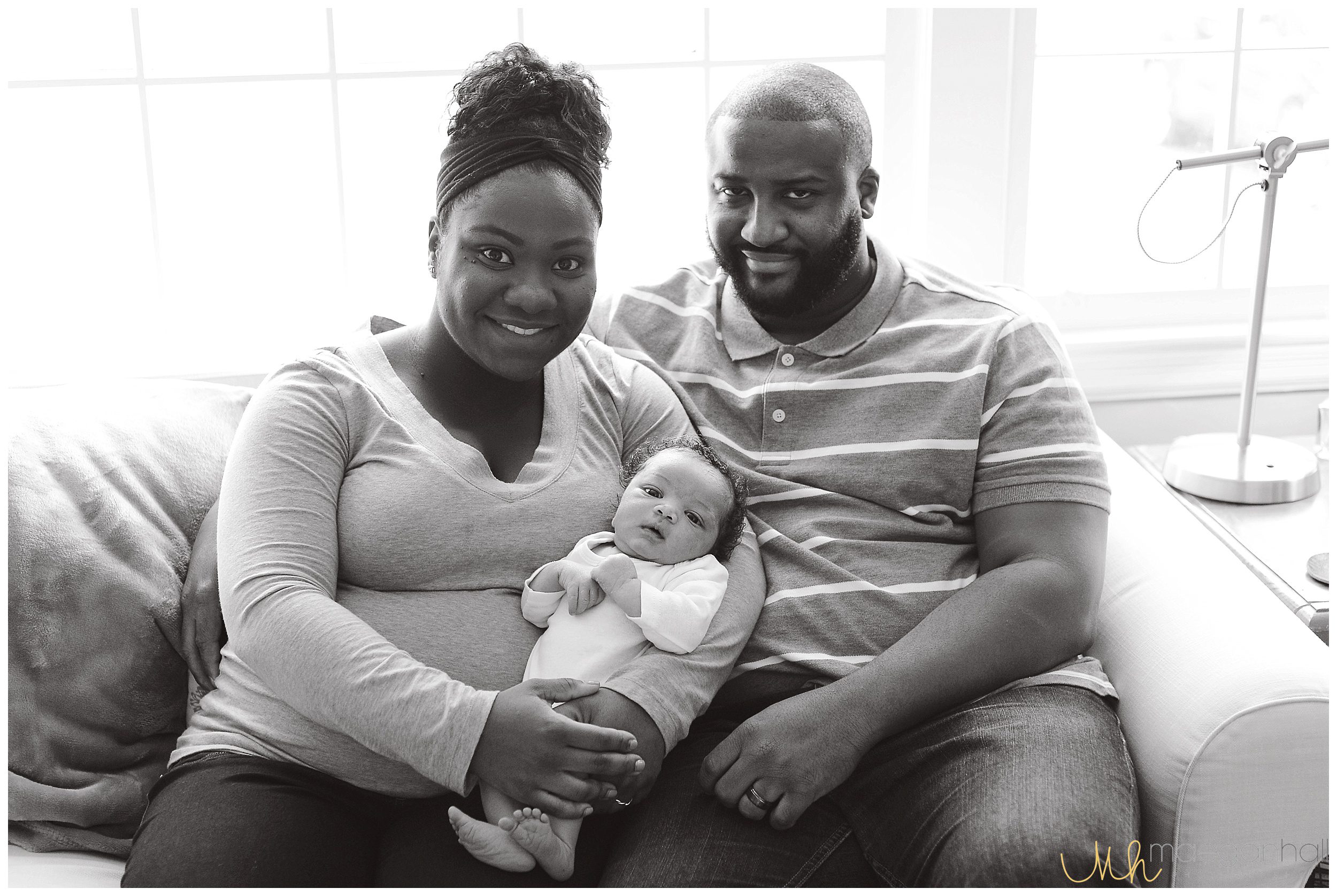
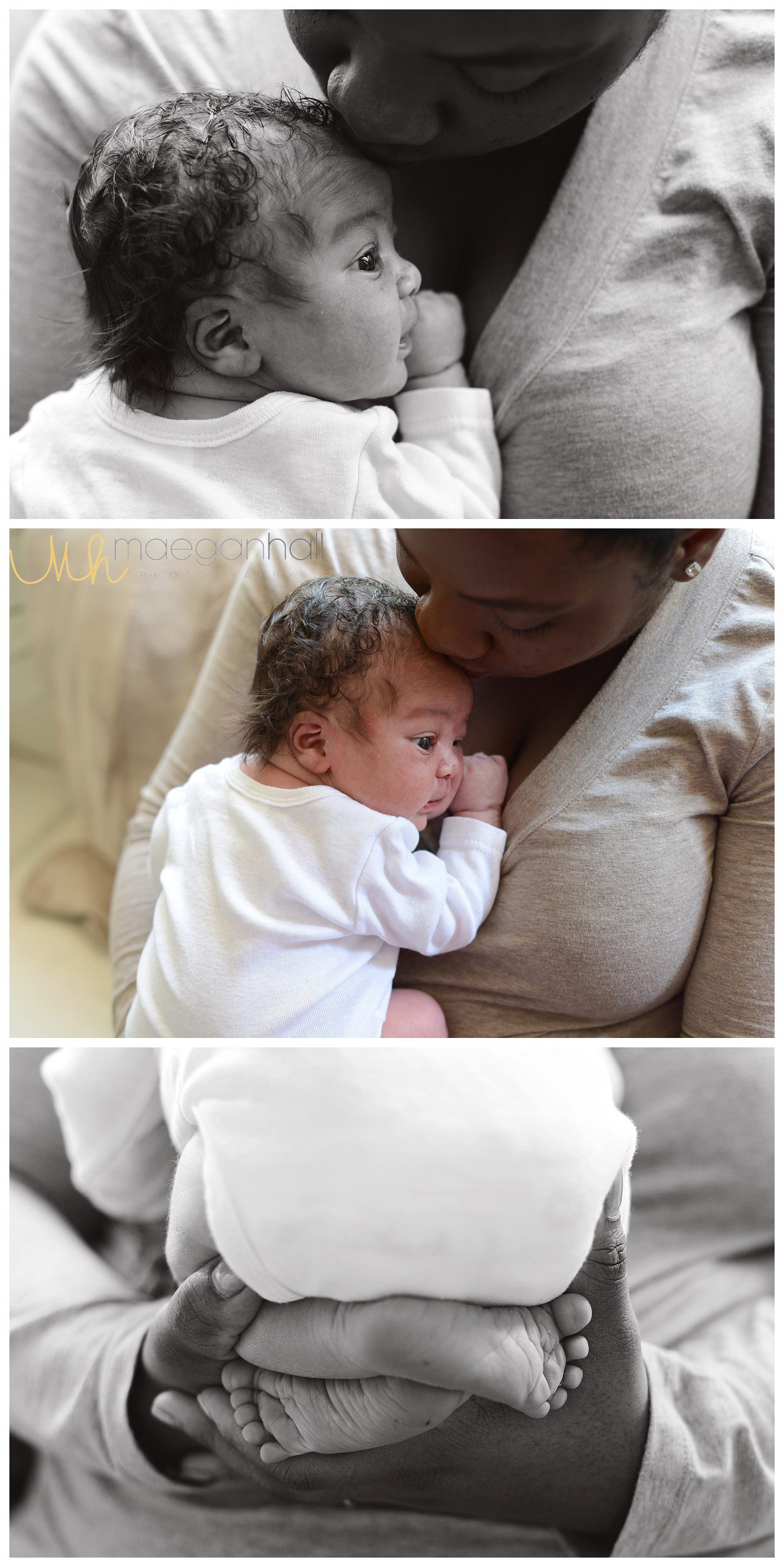
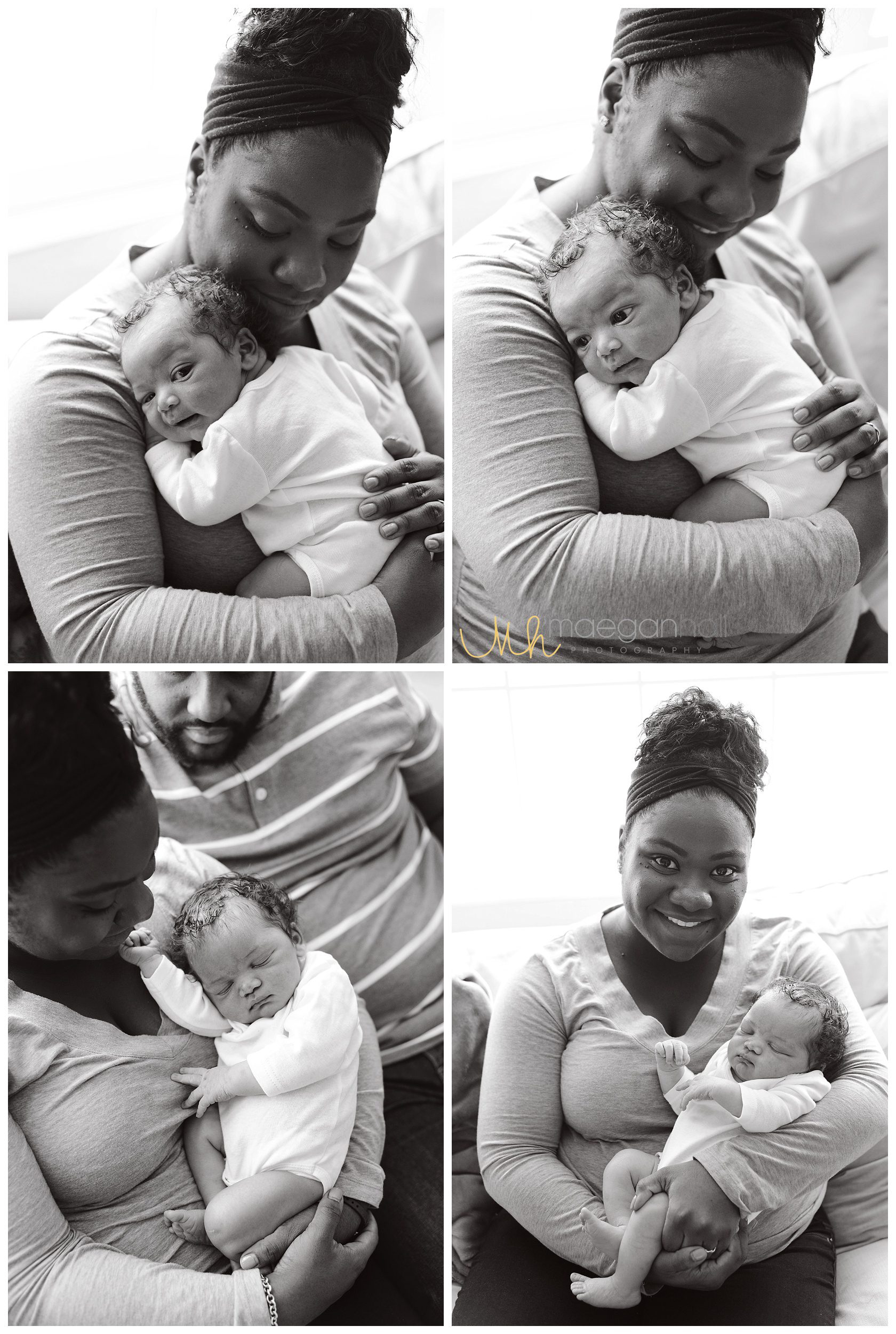
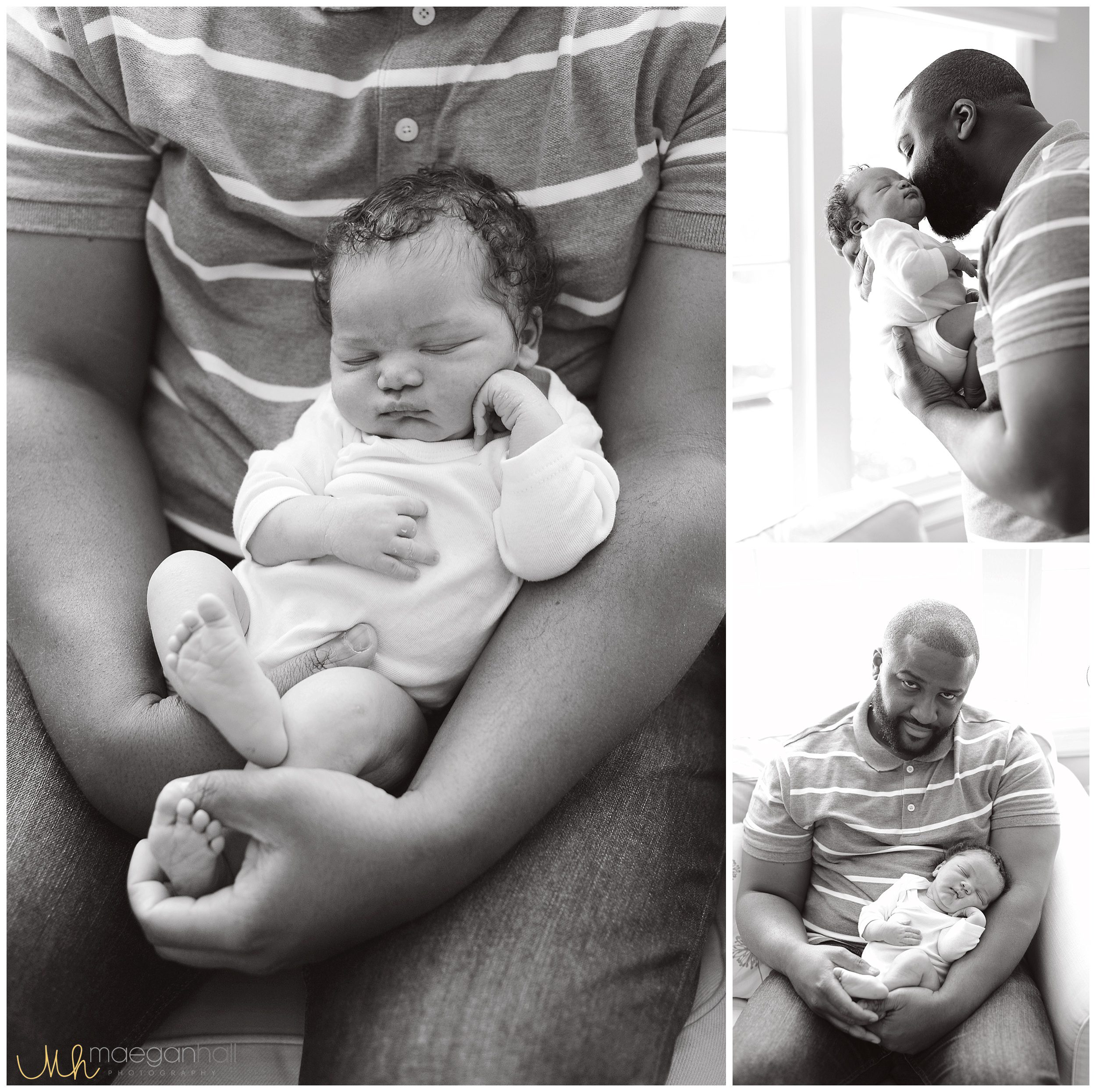
Approximately an hour or so later Caleb was born on Friday April 7 at 2:55 p.m., all 9 POUNDS 6 OUNCES in what was a calm, peaceful and enjoyable environment. Corey and I were both there and awake, talking and joking with Dr. B and the nurses, able to see and take pictures of everything and our skin to skin request and delayed cord clamping was honored perfectly.

Afterwards Caleb’s oxygen level was below what it should have been (likely a result of being in distress inside) so they took him to the NICU. Thankfully Corey was able to be by his side the whole time while I went into recovery. He stayed a day and a half then joined us in the hospital room and perfectly completed our new family of three.”







