Atlanta Birth Photography
Postpartum Depression Series: Kathryn
I’ve been meaning to start this series for awhile, but it takes time for mom’s to be in a position to discuss things they’ve worked through. The timing needed to be right and these brave moms are starting to come forward.
This is me, and this is my story.
I am lucky. I’m here and not there. I can write my story today because I managed to get some help. Some are not so lucky. They are there. They died of suicide. Here is my story. I hope you listen.
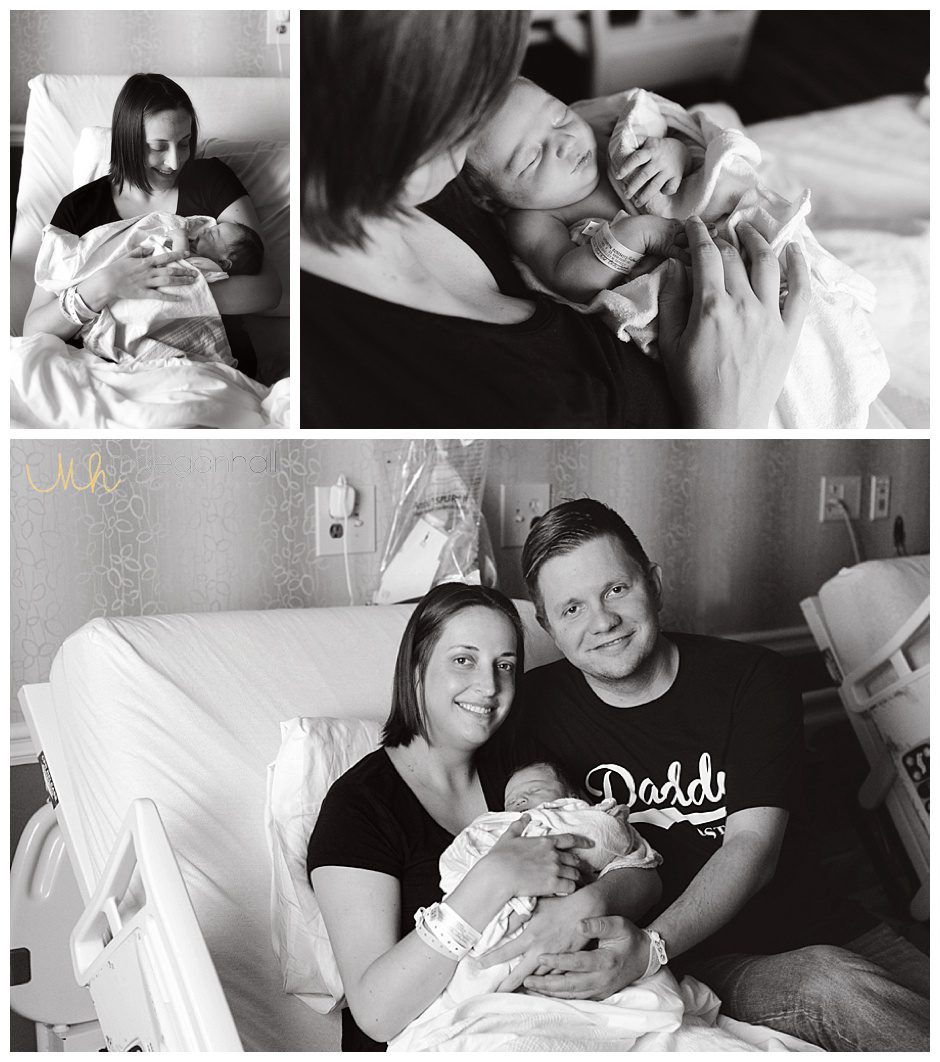
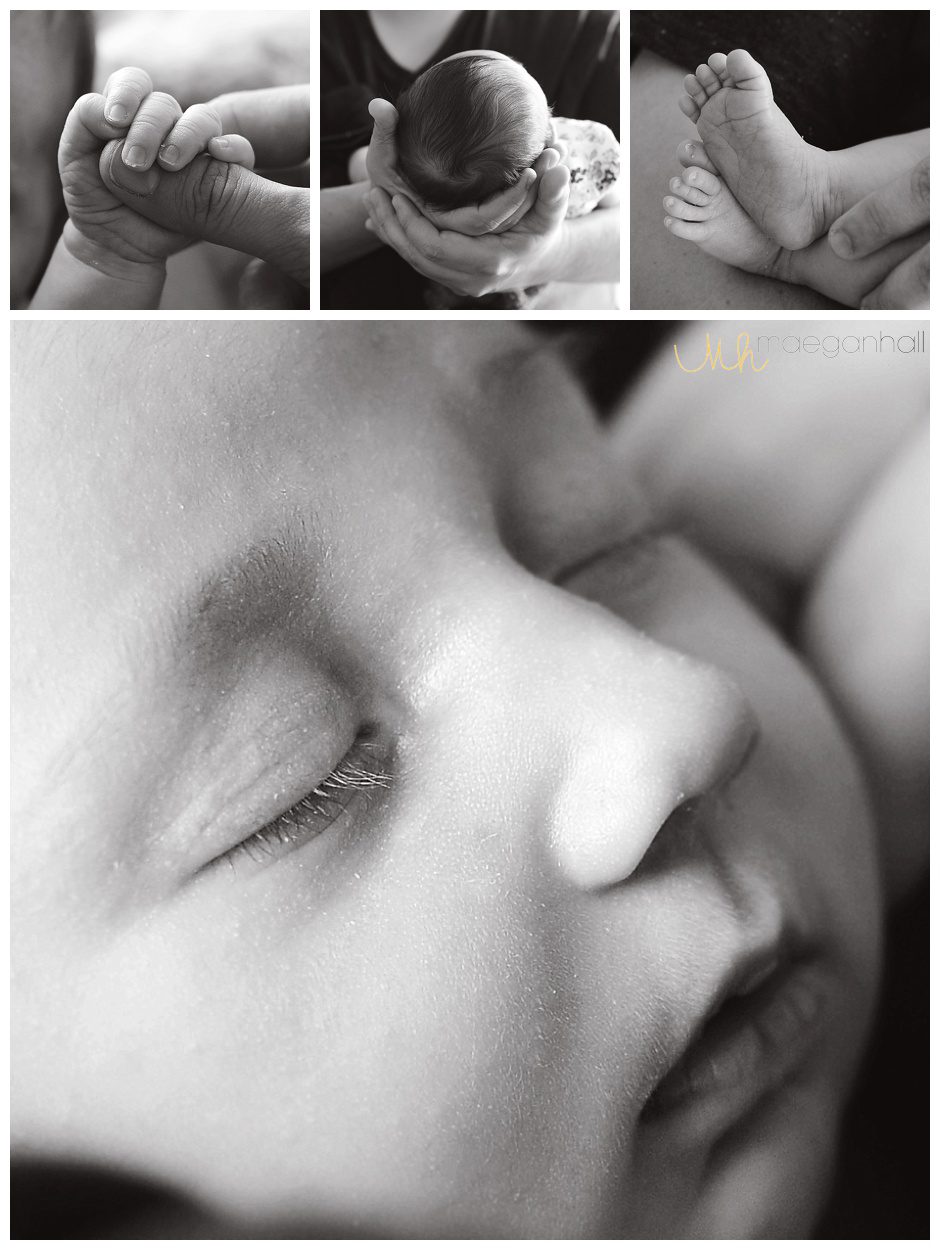
I really don’t know where to begin. I am scared of reliving the past – the guilt and shame were excruciating. I was numb but cried (what seemed like) all the time. One of the few things I remember is feeling like a monster for not falling in love with Alexandra the moment she left my body. As I write this, I am fearful of people’s judgement, especially other moms.
I experienced postpartum depression (PPD) and anxiety (PPA) after delivering Alexandra. I knew little about these conditions despite having dealt with depression at a younger age. Little did I know that because of my medical history, I had an increased risk of experiencing depression and anxiety during and after pregnancy.

Looking back on my state of mind during my pregnancy, I likely had perinatal anxiety (anxiety while pregnant). I know, you’re thinking, “all pregnant women have anxiety.” Yes, I agree, many (if not most) have anxiety to a certain degree. Pregnancy, birth, and motherhood are all reasons to experience at least a little anxiety.
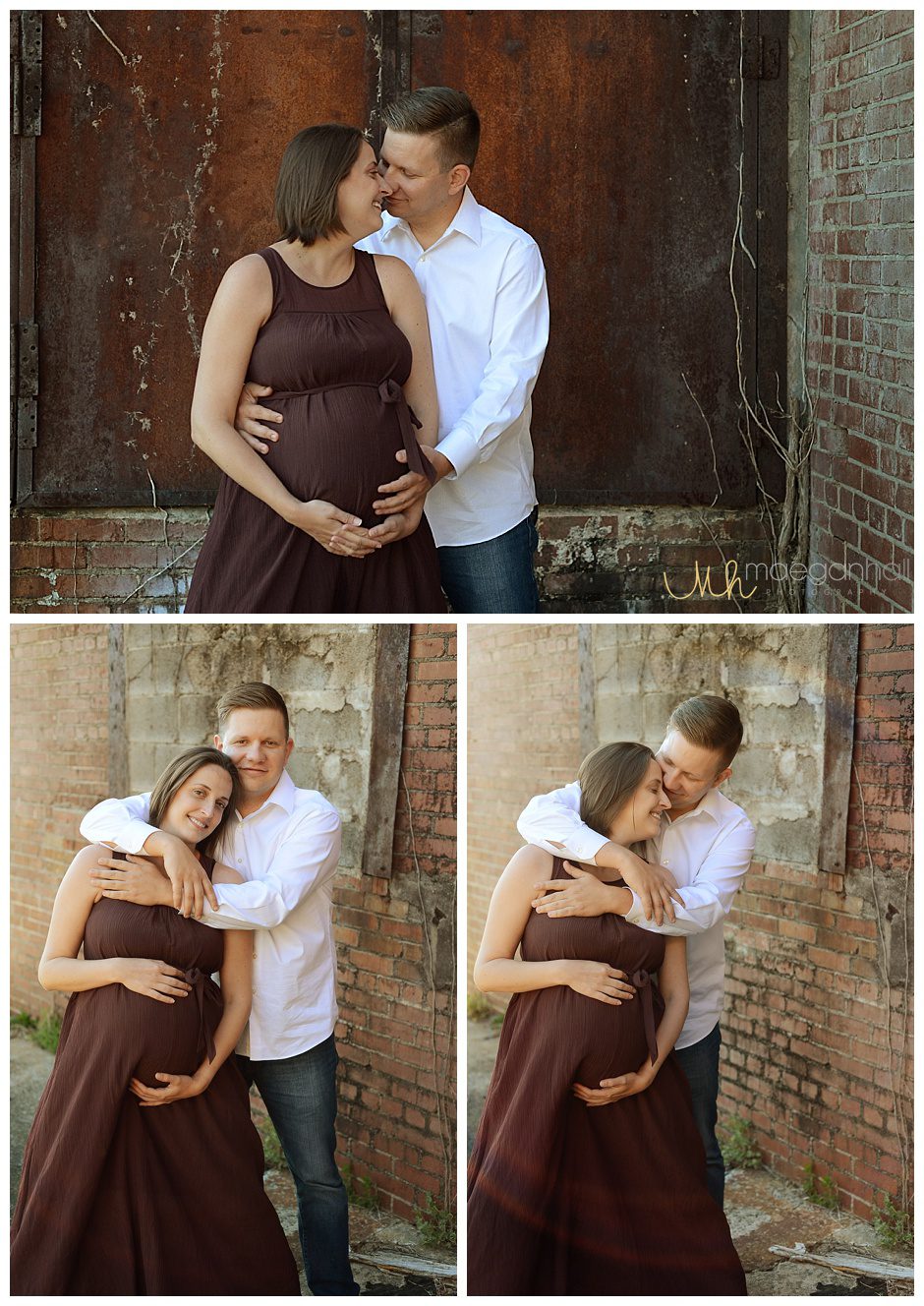
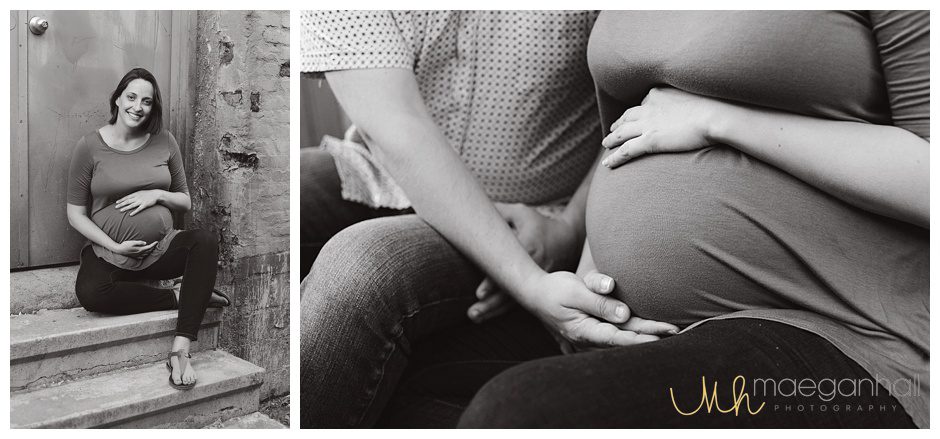
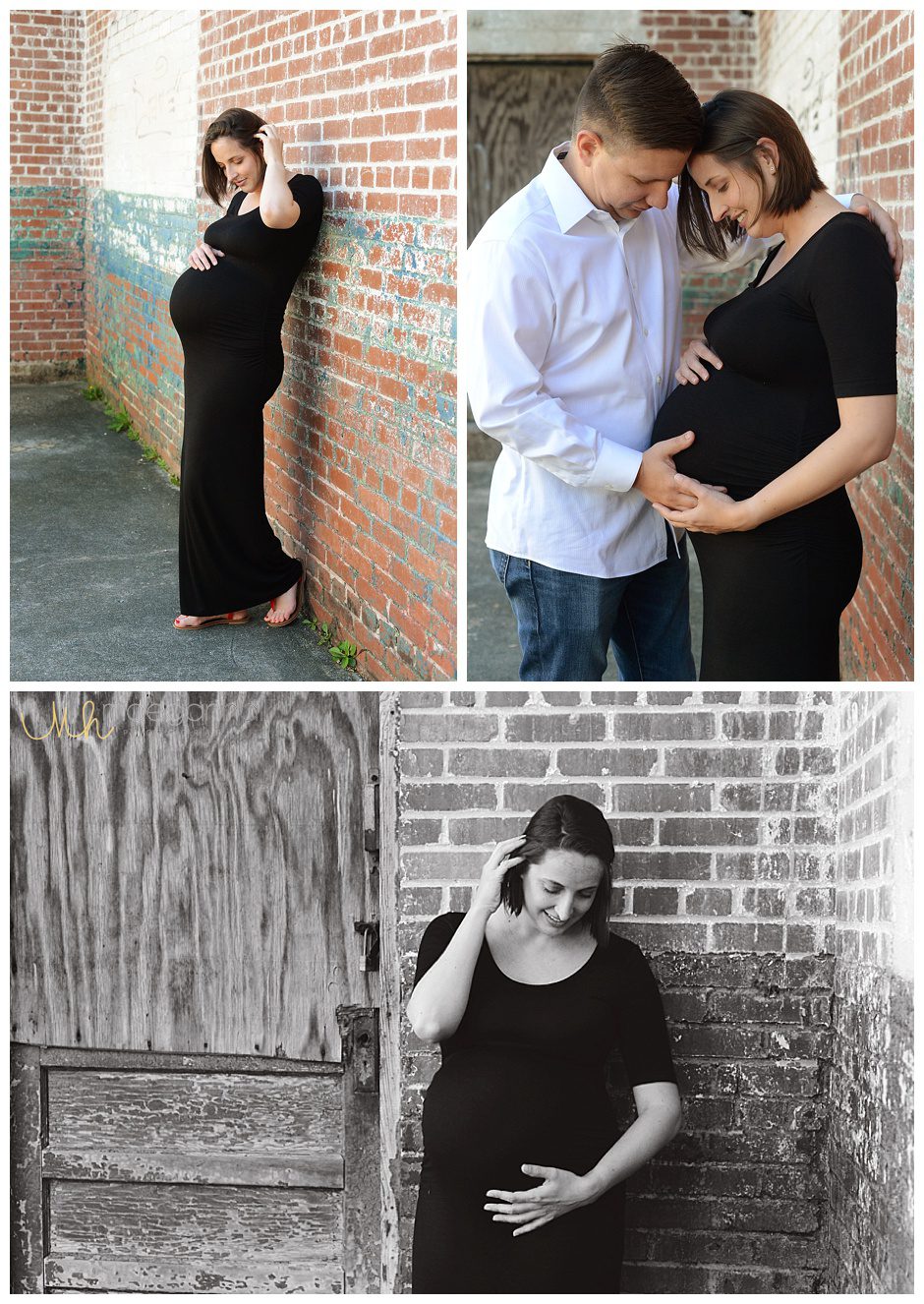
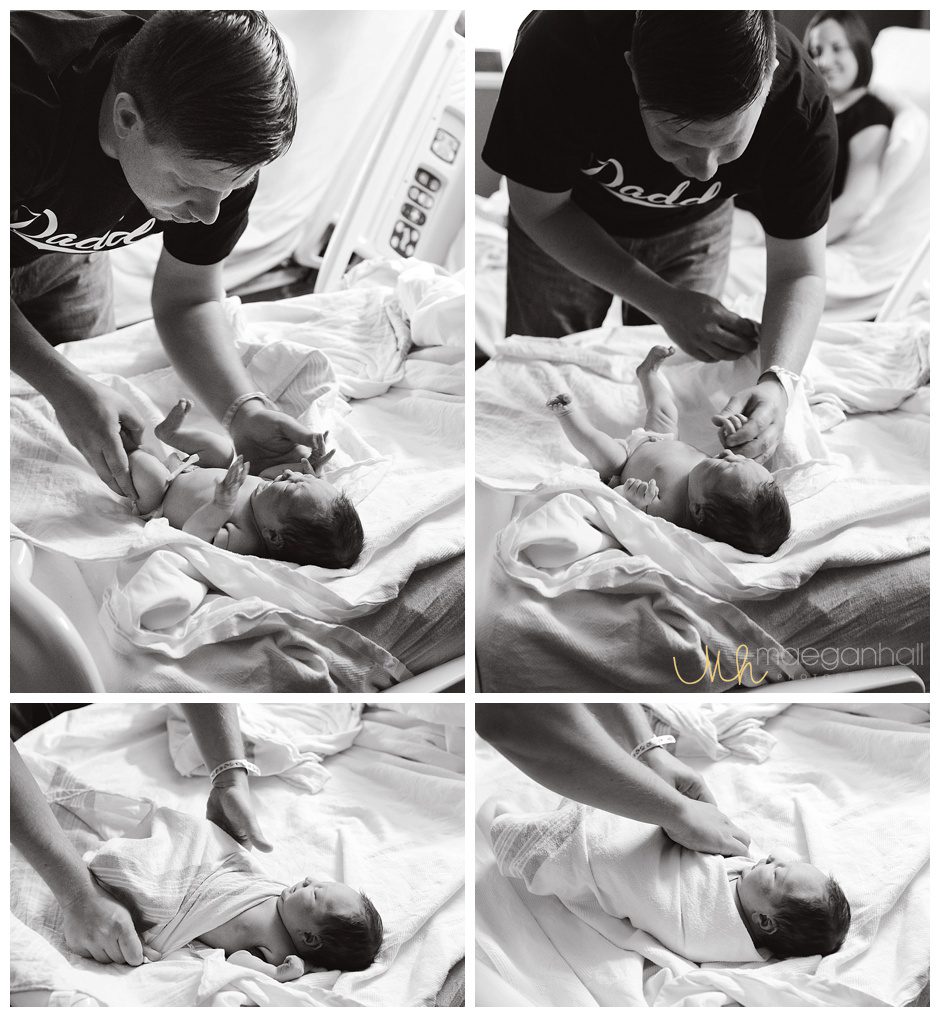
I was the quintessential first-time mom-to-be. I attended a birthing class (hypnobirthing to be specific), a water birth course (I wasn’t sure but wanted the option), lactation session (because apparently breastfeeding is hard), went on two hospital visits (exposure therapy for Pat – he is squeamish), and had two doulas (one of whom was a photographer for those grisly yet awe-inspiring birth pictures).

I saw a midwife throughout my entire pregnancy, and Alexandra was delivered by my midwife. I selected my hospital based on a couple of factors; the main factor was the cesarean birth rate of first-time moms.


I was interested in the rate among first-time moms specifically to control for moms who were having a second cesarean following a prior cesarean birth based on medical recommendations. Other factors included whether water both was an option and whether hospital policies were mother-baby friendly in the event of an uncomplicated birth.
I had researched and made (in conjunction with Patrick, of course) all critical decisions prior to the last month of pregnancy, such as whether Alex would get a vitamin K injection, hepatitis B vaccine, and antibiotic eye ointment.

We had also considered several different scenarios that presented different choices, like if my water didn’t break naturally, when would I let them break my water using the “hanger” (just kidding…kind of – it’s more of a hook).

Nonetheless, I just wanted to let my body do its thing and keep my mind out of the way (it’s been known to interfere a time or two). I also wanted to avoid any unnecessary medical interventions because one medical intervention increases the likelihood of needing a second medical intervention.

I was trying to avoid my biggest fear of pregnancy and birth – bleeding to death. Did I mention I took out a fairly substantial life insurance policy because I was convinced that, despite my low risk of bleeding to death given my demographics and risk factors, I knew I was going to bleed to death, and my new baby girl and husband would be here without me. All very normal concerns but my reactions may not have been so normal (whatever normal is).
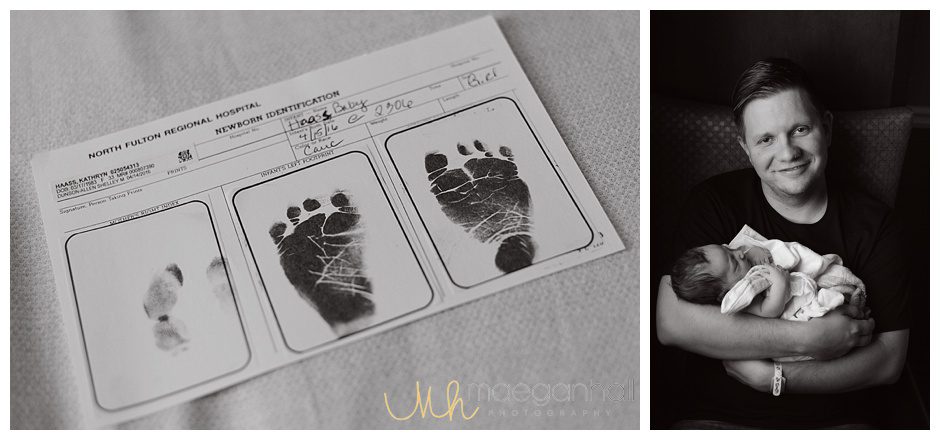
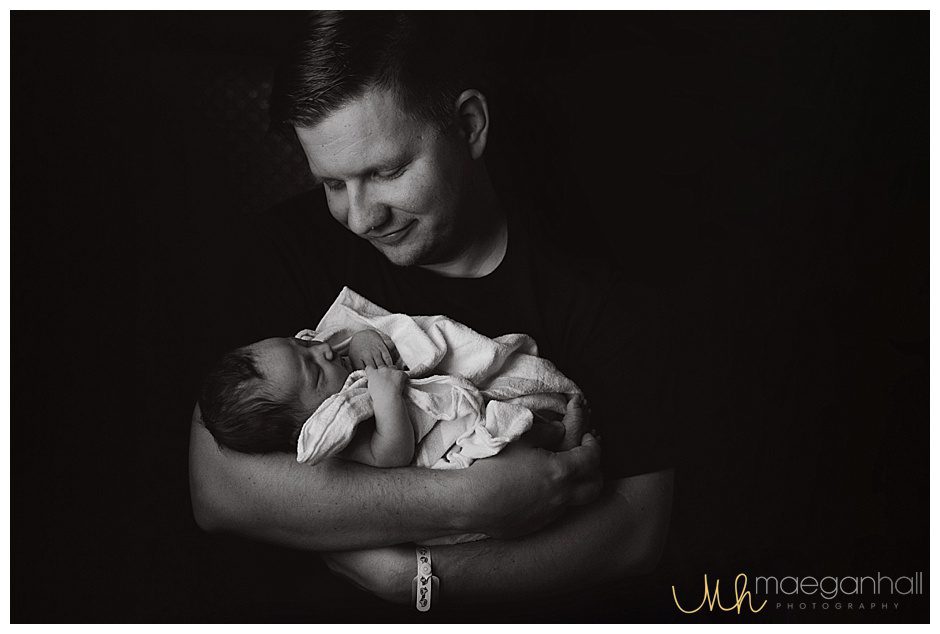
Alex entered the world as gentle as possible. I had an epidural—one medical intervention–but that was it. And I did not bleed to death. My insurance classified her birth as a “simple delivery”, despite the $29,000 price tag. While I had prepared for everything within my control to that point in time, what happened next was unexpected and I was completely unprepared.

Over the next three months, I lost all my ‘baby-weight’ and an extra ten pounds. I was officially under-weight for my height. I was sleeping at least eight hours, although not consecutively. This is practically unheard of for new moms. I know you are thinking, “B****!” I was back at work, and apparently thriving (according to my boss) despite having to leave my daughter at daycare.

Here is what actually happened. I wasn’t eating but I was still pumping a liter of breastmilk a day. Despite all my breastfeeding efforts, my cycle started three months almost to the day after giving birth. Oh yeah, I had extreme pain when breastfeeding so I exclusively pumped which increased my supply beyond what Alex consumed daily. However, I was unable to freeze my milk due to lipase (google it – I still don’t know).
I slept whenever I could – when Alex slept and when my husband or anyone else was home. I slept instead of eating, going outside, doing laundry or dishes or anything really. Despite all the sleep, I was still exhausted.
I had pain while breastfeeding and pelvic pain for six months after birth (none of which could be explained by my or any doctor). I began to drink wine, sometimes too much. (Stop judging me…I pumped and dumped.)

I cried frequently—several times a day, at work, at home, in the car. They called it the baby-blues. No, this isn’t a lullaby. It is a horrendously inaccurate term used to invalidate feelings a woman has after birth. I was still ‘blue’ after six months. I reached out to my midwife, a lactation doula, a co-worker, and employee support staff at work to get help for what clearly was depression (postpartum – within one year of birth).
My feelings were repeatedly dismissed. I was given a number of disheartening excuses for why I could not access (or didn’t need) help:
“You are not pregnant anymore. We cannot see you.”
“Well, it looks like you are doing everything right. I’m sure you will feel better soon.”
“Your depression cannot be that bad or debilitating. You still come to work every day.”
“But you look great! Look how much weight you have lost.”
At nine months postpartum, I was at work and I broke. I called Patrick and he met me at work. We called the suicide support hotline from the parking lot, not because I was actively suicidal, but because I was in crisis and needed some type of intervention. I had tried for five months to get help of any type, but no one would listen.

I spent the next three days as a patient in a psychiatric ward. This floor specifically dealt with people in crisis. While I was in a crisis situation, I suffered from postpartum depression and anxiety, conditions not taken seriously and largely misunderstood. I was released and readmitted again less than one month later. I then spent two weeks in-patient at University of North Carolina (UNC) Center for Women’s Mental Disorders.
My daughter is three and a half now. I’ve had time to heal and reflect, and reflect and heal some more. I don’t have PPD or PPA anymore, mainly because the medical system changes your diagnosis after one-year postpartum. I am still healing from the aftermath of depression and anxiety after I had Alexandra. Also, probably more so, I am still healing from the horrors inflicted by peoples’ misunderstanding and harsh words, our society’s stigma around mental illness, and this country’s medical system that lacks a sound mental health infrastructure.

So now what? Why am I telling my story now? It’s been three and a half years since my daughter was born and about two years since I was able to even speak of my experience. Even now when I speak about my experience with PPD, PPA and what might have happened if I didn’t get help, I tear up.
Two weeks ago, I received an email at work about the passing of a co-worker. He died of suicide. While his story is possibly quite different from mine (I don’t know his story), we likely shared similar feelings of hopelessness. Maybe sadness over the situation and frustration that the solution and help was so hard to find. I realized one difference; I am here and he is there. I can speak out and bring light to a dark place.
Everyone has their own experience. Despite how we arrived at that dark, lonely place, we should all be able to get help. He wasn’t able to get help and that is not his fault. I decided that day it was time to share my experience.
I want to reduce stigma, increase awareness, and develop a wider conversation about perinatal and postpartum mood disorders. But I also want to start an inclusive conversation about mental health and access to treatment to prevent people dying of suicide.
I guess sometimes you need money to that, but money is not my primary goal at all. If you want to contribute, please click the link to my fundraiser.






