An HBAC is a Home birth after having a cesarean.
Is it safe? What exactly are the statistics?
HBAC: Home Birth After Cesarean – FAQs & Stats
Many families who have had a cesarean wonder: “Can I give birth at home next time?” For many families, an HBAC (Home Birth AFter Cesarean) can be a safe and empowering choice. Still, it’s normal to have questions, especially when statistics, and personal fears get tangled together.
As an Atlanta birth doula photographer, I’ve witnessed countless families navigate this decision. Below, you’ll find some of the most common HBAC questions, along with data, insights, and encouragement to help you explore whether this path is right for you.
I asked a FB birth group, “What questions do you have about VBAC at home?” I took your questions and approached 3 specific, local women with these questions.
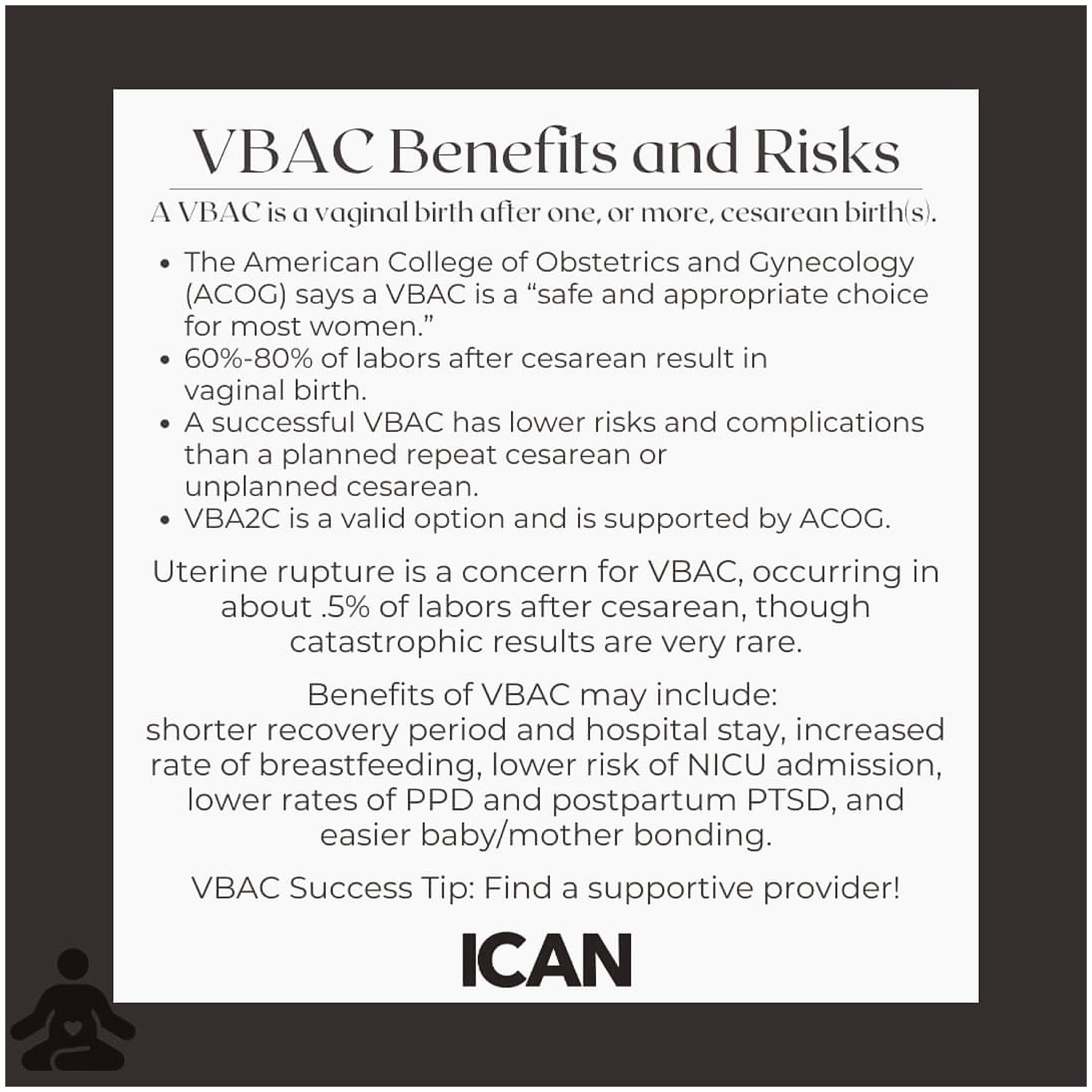
Here are the stats we know according to ICAN of Atlanta!
ICAN of Atlanta is the Atlanta chapter of the International Cesarean Awareness Network, a nonprofit organization whose mission is to improve maternal-child health by preventing unnecessary cesareans through education, providing support for cesarean recovery, and promoting Vaginal Birth after Cesarean (VBAC).
What Is HBAC? Home Birth After Cesarean
HBAC stands for Home Birth After Cesarean. It refers to families who choose to labor and give birth at home following a previous cesarean delivery.
For many, this choice comes after being told “once a cesarean, always a cesarean.” But modern evidence shows that vaginal birth after cesarean (VBAC), including at home, is possible for many families.
Meet the experts:
Cassia Beckman – ICAN (International Cesarean Awareness Network) Atlanta Chapter Leader. VBAC + HBAC mom herself.
Shoshanah Blaiss – MSN, CNM, IBCLC, Owner of Binah Birth and Breastfeeding. Also a VBAC + HBAC mom herself. She is pictured as the midwife below.
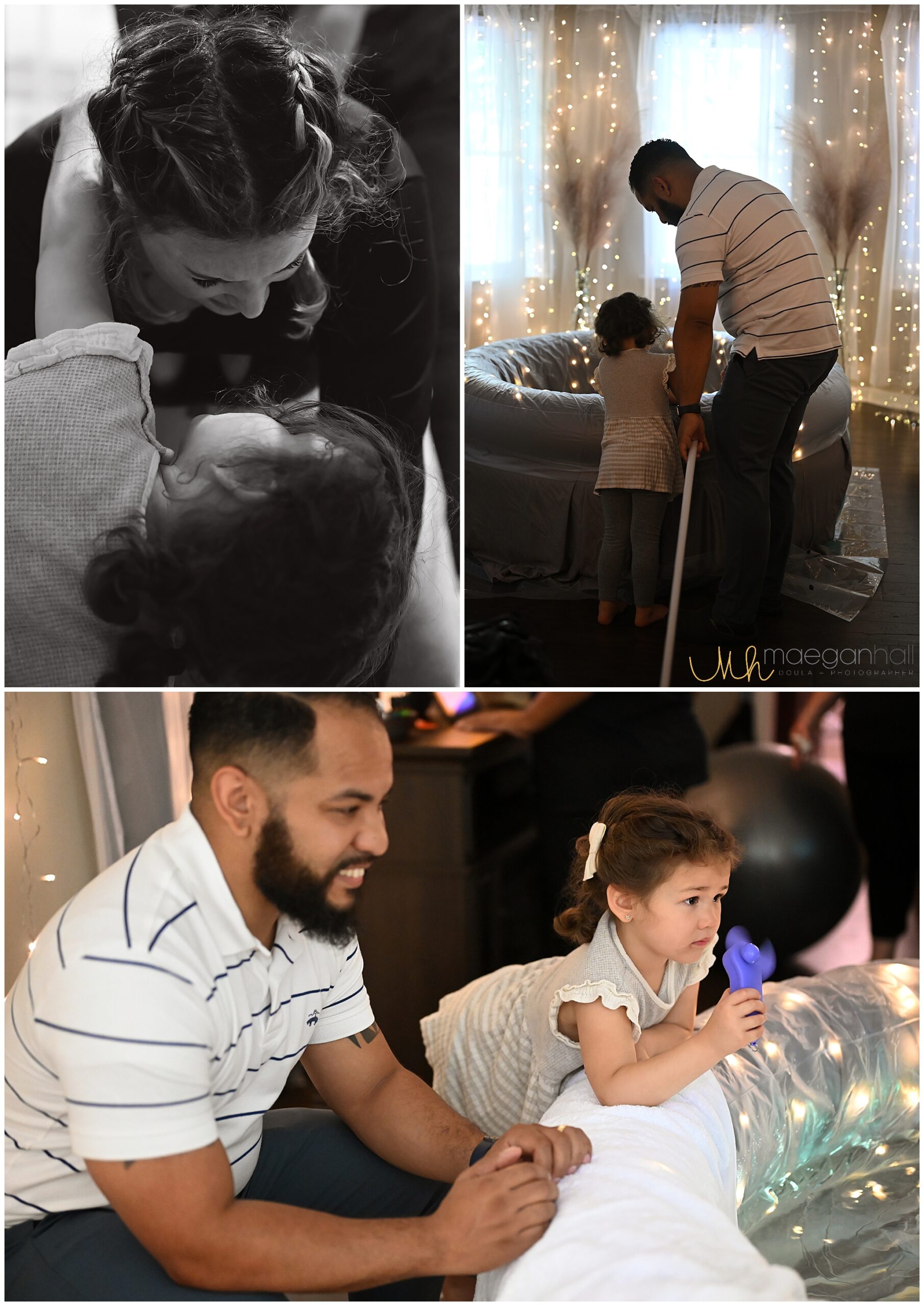
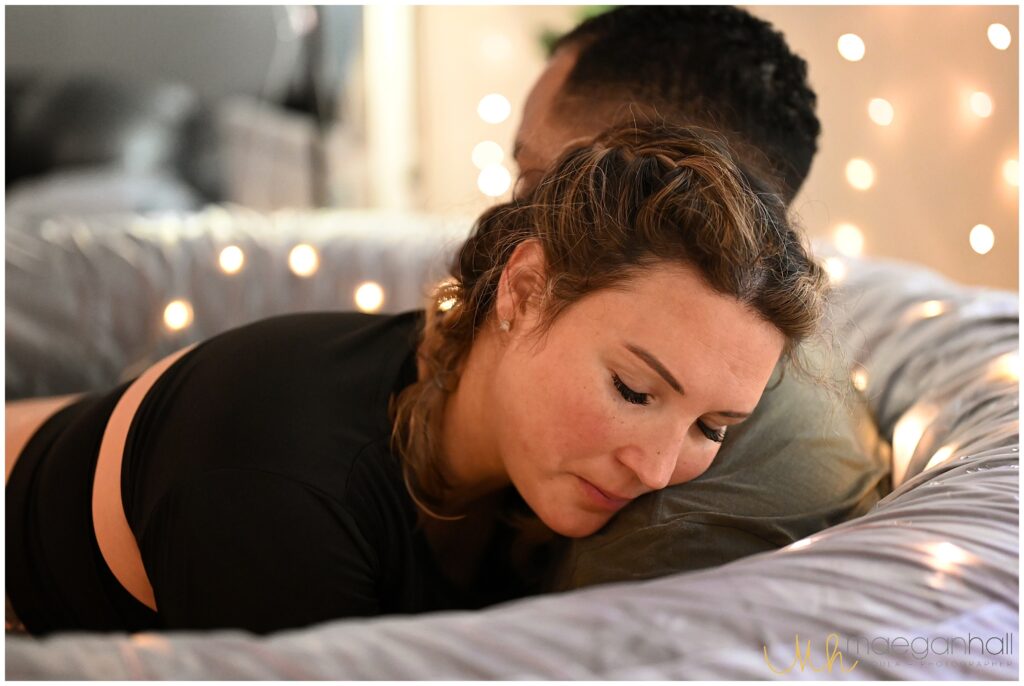
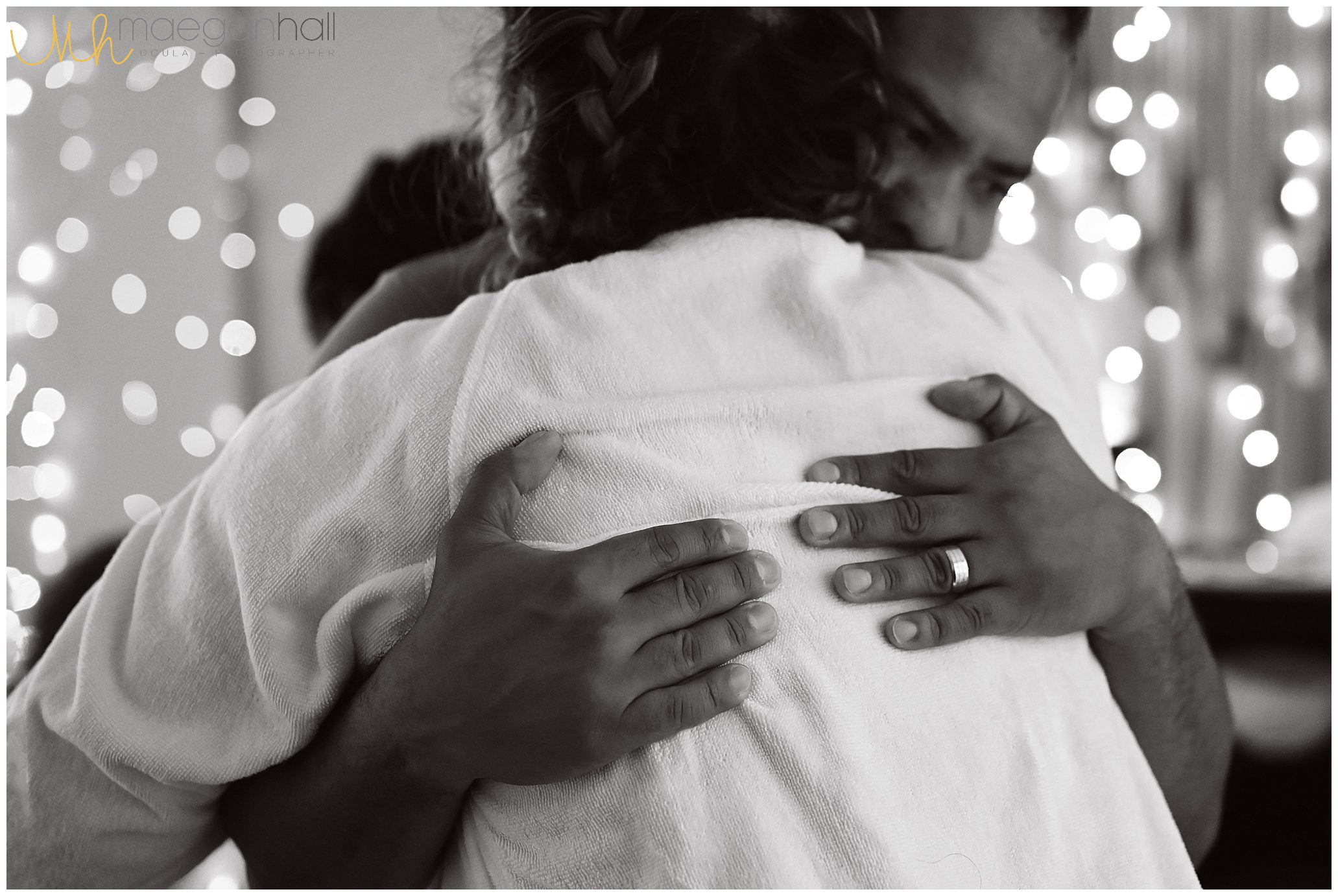
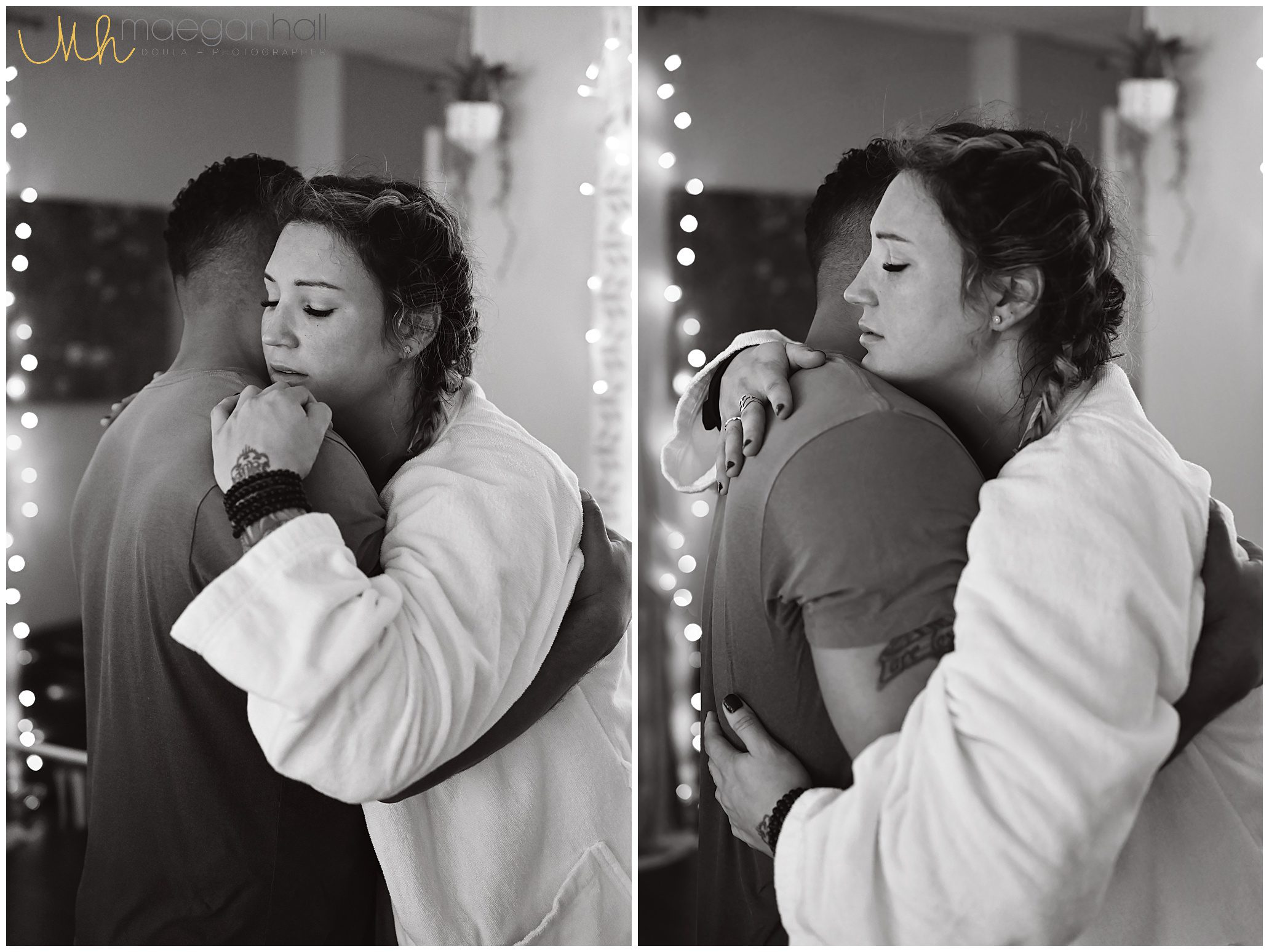
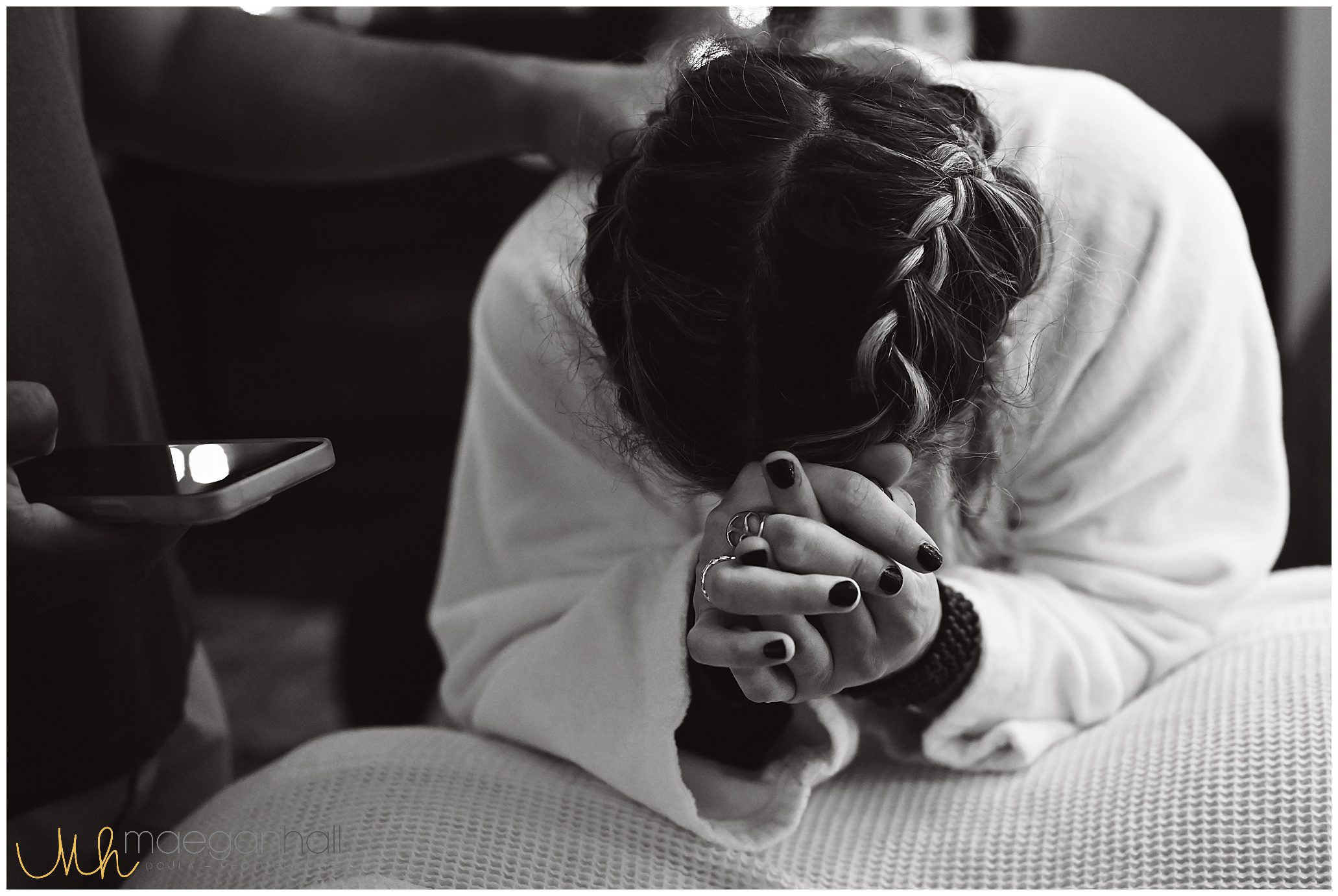
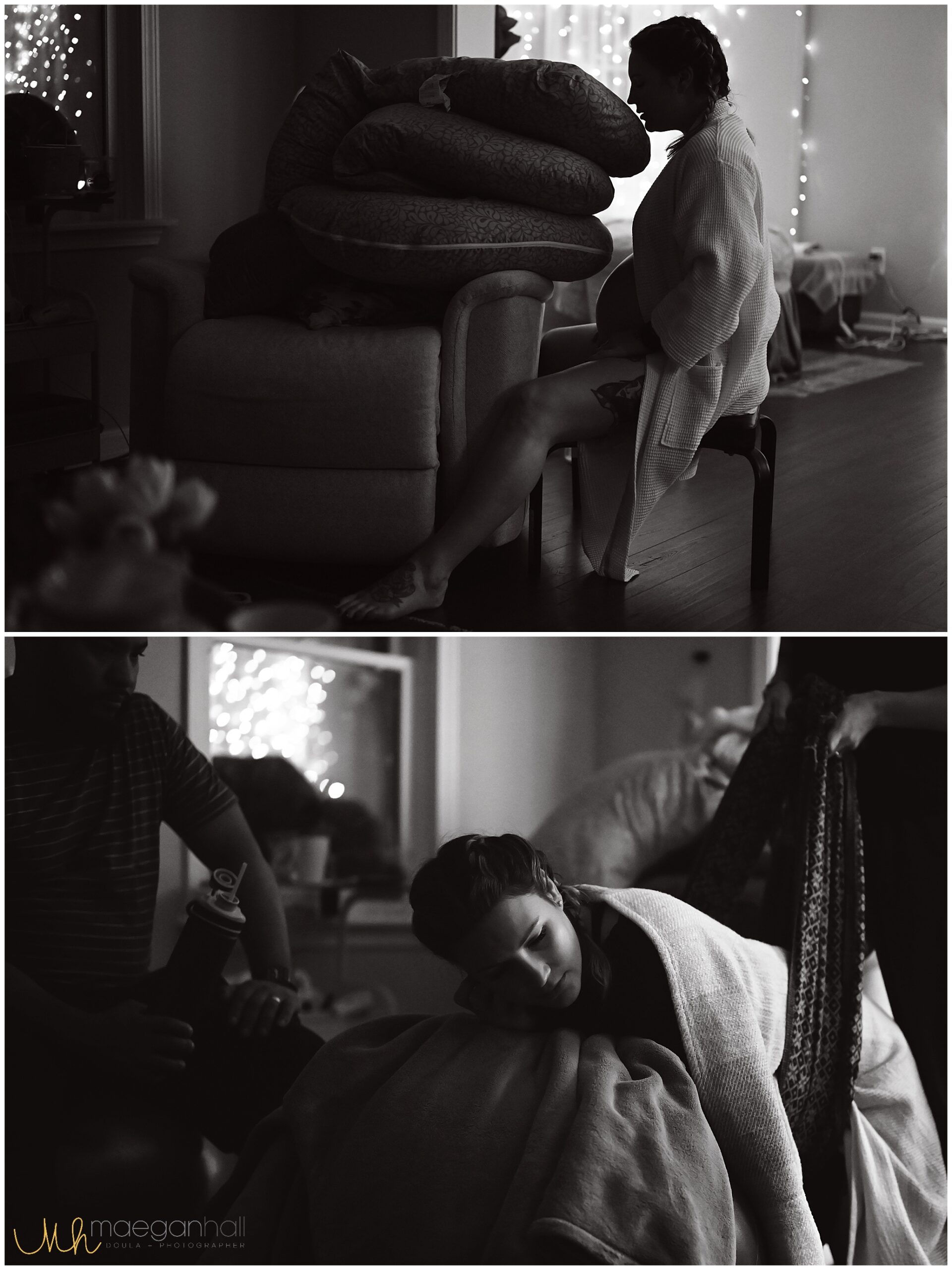
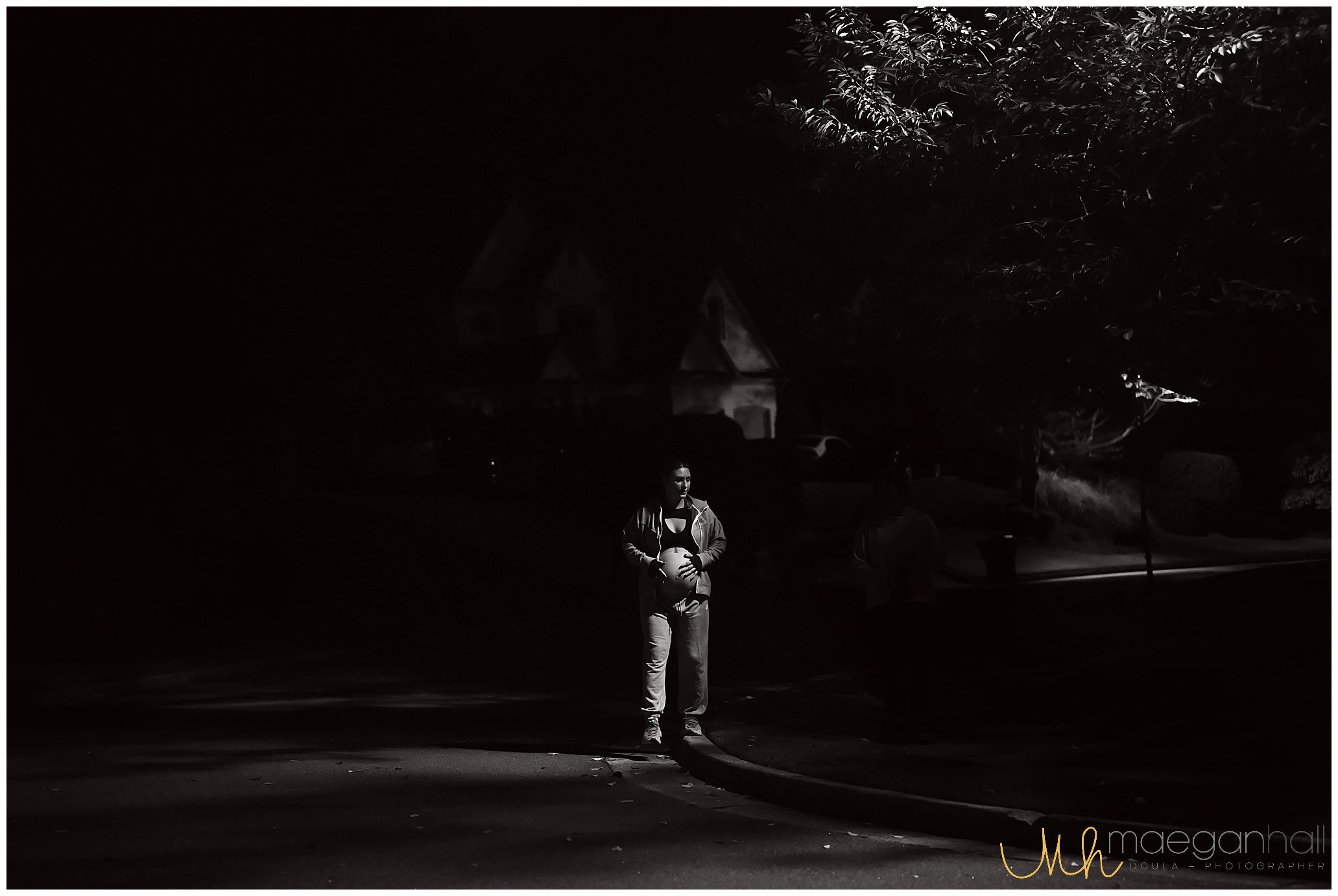
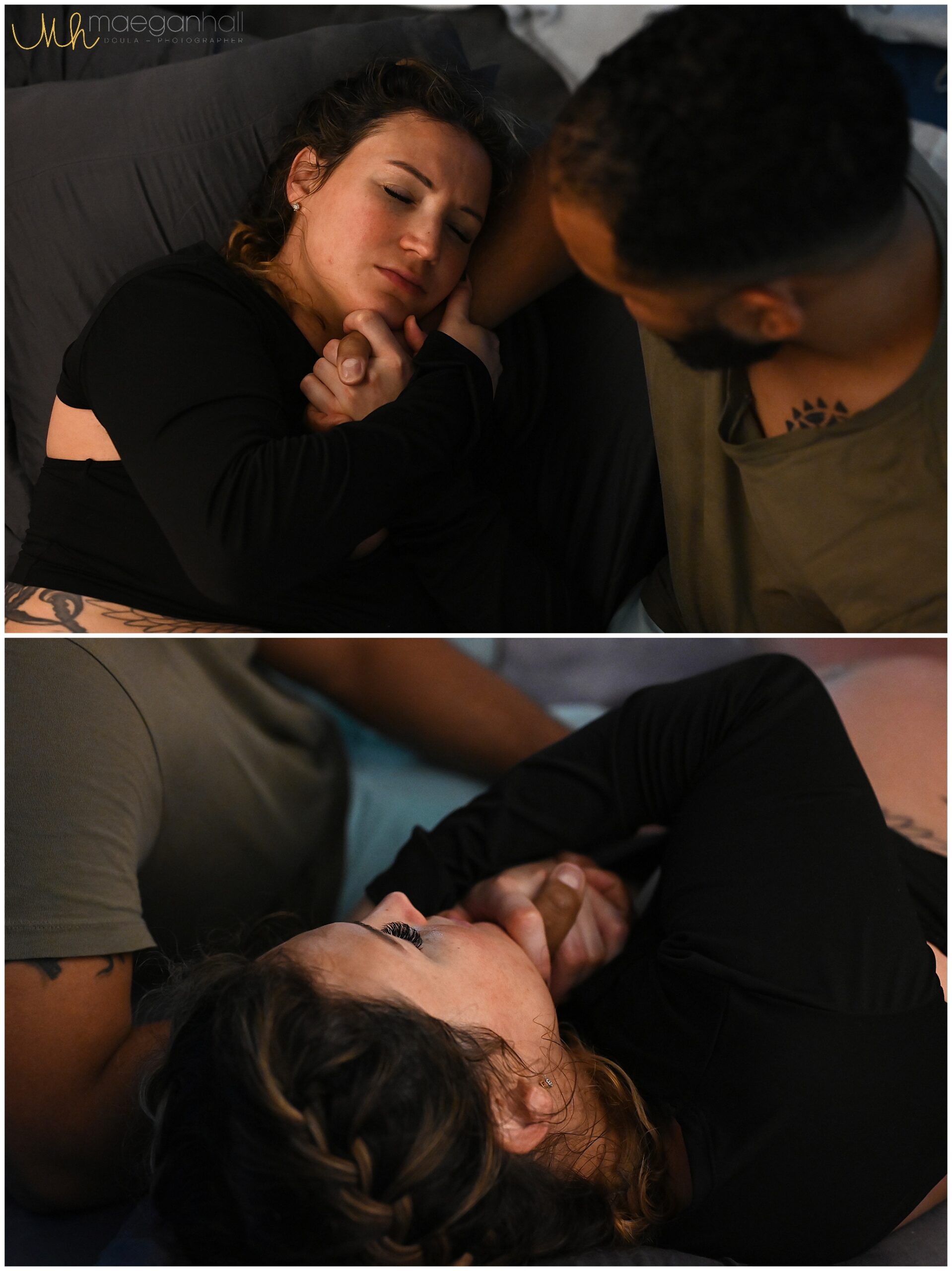
Caroline – mom to two girls, and recently chose to have her first HBAC (VBAC at home). See her birth photos throughout this post.

**Special mention: Cassia wrote an extensive paper for this blog post. All the delicious studies, #s, stats and facts for us nerdy types. For the purpose of quick tips in easy-to-understand language, I will reference that paper. If you are interested in her exact research, please read it HERE

Is HBAC Safe?
This is the first question most families ask. Research shows that a planned HBAC can be safe for carefully screened candidates, especially when supported by a qualified midwife.
- Studies indicate that around 60–80% of women attempting VBAC are successful in having a vaginal birth.
- The primary risk associated with VBAC is uterine rupture, which occurs in less than 1% of cases. Midwives are trained to monitor for warning signs and transfer care if needed.
- Planned home births are best suited for families who are otherwise low-risk and who are supported by skilled providers with clear hospital transfer plans.
Every family must weigh personal risk tolerance, medical history, and provider guidance when making this decision.
What do you want people to know about HBAC?
Cassia, “First – we need to recognize that there is no risk-free way to birth. None. Not vaginal. Not cesarean. Not VBAC. Not repeat cesarean. Not HBAC. There are risks to every. single. option. So often, when we talk about birth after cesarean, we focus on the risk of uterine rupture. I think the unpredictability makes uterine rupture feel more menacing and more common than it really is, much in the same way that many people get more nervous when traveling by air than by car.
For more information about looking at risk, I highly recommend reading the articles on SmartBirth.org. That site was created by a nuclear engineer who realized a lot of us don’t have good experience with evaluating risk.”

Shoshanah, “HBACs are both incredibly special and also very ‘run-of-the-mill’ births. I don’t treat my HBAC clients differently than my non-HBAC clients. Everyone deserves to be met where they are & treated as an individual. However, there is something extra special about the ‘I did it!’ moment of an HBAC – especially a first one. It’s an honor to witness that moment of triumph!”
Caroline, “Have a plan and prepare for it! Interview midwives immediately, they book fast. Prepare your body – eat well, yoga, pelvic floor PT.”

Why Do Families Choose HBAC?
Families often consider HBAC for emotional, physical, and practical reasons:
- Avoiding repeat surgery and its longer recovery period
- Desire for a natural, unmedicated birth
- Creating a calm, family-centered environment
- Taking back autonomy after a difficult or traumatic hospital experience
For many, HBAC isn’t just about the mode of birth — it’s about rewriting the story of how their baby comes into the world.
Do you know any of the stats on HBAC? Success rate?
Cassia, “All of the studies found that those who planned HBAC had a higher chance of actually having a vaginal birth than we see for planned hospital VBAC. The UK study directly compared planned HBAC to planned VBAC in the hospital and found the rates of vaginal birth at nearly 88% HBAC vs 69% VBAC.”

How Can I Prepare for an HBAC?
Preparation is key. Here are a few practical steps families take:
- Gather your records. Bring operative and prenatal reports from your cesarean to your midwife.
- Choose your team wisely. Surround yourself with providers who believe in your ability to birth.
- Plan for both outcomes. Prepare mentally and practically for home birth and for a possible hospital transfer.
- Hire a doula. Continuous labor support can make all the difference in navigating fears and staying grounded.
How can someone start prepping their body now (after birth) for when they are ready to
conceive again?
Cassia, “We all know the recommendations to improve health – eating a nutritious diet with a variety of fruits and vegetables, intentional daily movement, making sure to get sufficient sleep, strengthening relationships, reducing stress. It can be really hard to get all, or even some, of those in, especially when in the thick of parenting a baby or young child. But every step we take toward improved health also improves our body’s ability to support a future pregnancy, if desired.”

Shoshanah, “Allow for an adequate amount of time for physical healing (ideally, at least 12 months for an uncomplicated surgical or vaginal birth). Make a preconception appointment with your midwife (or one you would like to work with) to screen for any underlying health problems or nutrient deficiencies, and evaluate for any lifestyle or other changes that may be helpful. This is especially important if you have been/are currently breastfeeding. Make sure your mind is ready! Have a plan for maintaining your mental and emotional health.”

What Questions Should I Ask My Midwife About HBAC?
When interviewing midwives, consider asking:
- How many HBACs have you attended?
- What is your transfer rate, and under what circumstances do you recommend transfer?
- What are your protocols for monitoring and safety?
- How do you collaborate with hospitals if transfer becomes necessary?
Having these answers upfront helps build trust and prepares you for every possibility.
What sort of emotional/psychological preparation should one seek between a traumatic cesarean experience and a VBAC at home?
Cassia, “It is really important to work through traumatic birth experiences, whether that birth ended in cesarean or not. And that is regardless of future pregnancy and birth plans. I think a lot of us end up trying to ignore, or forget, or otherwise bury the trauma endured, which can come from medical dangers or from the way we were treated (or both!). There is too often an idea (spoken or unspoken) that “all that matters is a healthy baby,” and that any bad experience with a birth should be completely overshadowed by the focus on the baby. It’s almost as if some think that expressing any negativity about the experience is somehow showing less care about the baby. But experiences are complex. When our baby is OK, we can feel both relief about that and can be sad or angry or otherwise troubled by the way things played out. And trying to ignore or bury a traumatic experience doesn’t resolve it – doing so only leaves us vulnerable to having future experiences trigger those feelings and memories.”

Shoshanah, “First, I don’t like the term ‘trial of labor’. No one’s body is on trial! Planning for a vaginal birth is planning for a NORMAL birth. A surgical birth is not a failure, it’s plan B (or C, or X, etc.), and any pregnancy can result in a cesarean, whether or not they have had one previously. Even if a cesarean wasn’t traumatic, the body remembers things the mind doesn’t always think about. My #1 recommendation is to join ICAN & attend the in-person meetings.”

Caroline, “Having a supportive midwife (and team) who understands your anxiety and your history. One who is willing to discuss concerns at length. Hypnobabies, but you have to actually do it!”

What sensations are normal around the incision during labor and pregnancy?
Shoshanah, “During pregnancy, some clients may feel discomfort/stretching in the lower pelvis, near where the external scar is. However, this is usually related to adhesions, ligament stretching, or general pelvic organ movement. For a client that had a typical incision (low transverse) for their cesarean, the location of the incision on the uterus isn’t typically the direct cause of any particular sensations due to its location on the lower part of the uterus.
In labor, most clients don’t report any noticeable sensation related to the incision, however, they may feel normal labor sensations (such as cramping or pressure) in the area of the scar.”

How Can I Prepare for an HBAC?
Preparation is key. Here are a few practical steps families take:
- Gather your records. Bring operative and prenatal reports from your cesarean to your midwife.
- Choose your team wisely. Surround yourself with providers who believe in your ability to birth.
- Plan for both outcomes. Prepare mentally and practically for home birth and for a possible hospital transfer.
- Hire a doula. Continuous labor support can make all the difference in navigating fears and staying grounded.
What driving distance from a hospital is preferred for HBAC clients?
Shoshanah, “I generally prefer that my HBAC clients are within 30 minutes of a hospital that has in-house OBs.”
Shoshanah, what can you do if a UR (uterine rupture) happens under your care?
“A suspected uterine rupture would be handled the same as any other obstetric emergency – rapid transport to the closest facility with obstetric services (determined prenatally). Because we plan ahead, we are able to call the hospital & provide a transfer report and a copy of the client’s prenatal records.
In an emergency, I prefer to accompany the client to the hospital. This allows me to continue to support my client & their partner, as well as make myself available to the receiving providers to answer any questions they might have.”

When is the best time to find an HBAC midwife (before ttc, while ttc, or while pregnant)?
Shoshanah, “I always think the best time to establish care is before conception, but that’s rarely what actually happens. I love to help my clients go into pregnancy with a healthy mind and body because that foundation is crucial to development in those early weeks. Prevention is one of the key hallmarks of midwifery care, and that begins BEFORE pregnancy.
It’s also a good idea to know if the midwife (you are interested in hiring) is planning time off in the next 12 months, so you aren’t disappointed if you conceive and then find out they won’t be available.”
Caroline, “As soon as possible! They book so quickly.”
Was your partner on board with birthing at home? If not, how did you both get on the same page?
Cassia, “By that point, yes. We both went through a process to get there. We had several births that left some trauma, had seen plenty of hospital policies that weren’t actually evidence-based, and had providers not be truthful with us. My birth right before was was especially troubling for me with the way things played out, both in labor and in the baby care afterward. And I was seeing several friends in the ICAN group have their babes put in the NICU for questionable reasons, with their family pediatricians later saying they didn’t think it had been necessary. Meanwhile, I was also seeing more stories about HBAC and starting to consider maybe checking it out.
That said, we didn’t expect to actually have a home birth, at least not at first. I had a lot working against me, and I chose the home birth route because I wanted to do whatever I could to stay healthy. I’d been told I had pre-eclampsia in the previous pregnancy, with the provider expressing how weird it was that I got it after several healthy pregnancies. At that time, low dose aspirin was not yet being recommended, so hospital providers didn’t have any preventative suggestions. They would watch for signs and then react as needed, but that was it. So I figured it wouldn’t hurt to try a more proactive provider and then transfer to hospital care if/when needed.
And my midwife was proactive! We talked diet a lot. She asked about my cravings and then identified a possible reason. For instance, when I was craving citrus she recommended adding some Vitamin C, and the cravings eased. It shocked me and made sense at the same time. She tested for more things on the urine samples, which alerted her to an early UTI and allowed her to help me address it quickly. She also caught when I had been so busy I’d forgotten to eat and gently reminded me I needed to care for me, too. She looked at food logs and encouraged some healthy adjustments. Her focus was on small course corrections to keep me on a healthy trajectory.
And it worked! I was surprised when it ended up being my healthiest pregnancy and I didn’t need to transfer after all! My husband was there with me in the interviews, and we discussed how we felt about each midwife afterward.
Additionally, the one we chose actually came to our home for appointments, so he was able to be there for part of the appointments as well. This helped him to build a relationship of trust with our midwife.”

Caroline, “He was after I showed him the research. He knew it couldn’t be any worse than the first time. We agreed I would be willing to transfer if anything went wrong. He was confident in my birth team. He prepared with me.”
What was your partner’s most comforting part of the HBAC?
Shoshanah, “The fact that we didn’t have to go anywhere. We were in the comfort of our own home.”
Caroline, “He loved that it wasn’t in a hospital!”
Was it difficult not having nurses the first 24 hours after birth?
Cassia, “No, but also yes. My midwife stayed for a while to make sure the two of us were OK and checked in again the next day. Sleeping without interruption was wonderful (no middle of the night routine checks). So I did not miss nurses in that way.
On the other hand, my husband was earnest but was busy with the kids. As this was my first time being home the first couple days after birth, and as I felt pretty good, I felt like I needed to do more than just rest. This led me to push myself too much.
When I planned an HBAC for the pregnancies that came after (that ended up hospital births for various reasons), I knew I’d need to do better planning for my own care for those first few days – I’d need to make it someone’s job to help me with food/water, etc, and to remind me to rest.”
Caroline, “The midwife came in the first 24 hours. The baby mostly sleeps! It was better at home because nobody was interrupting my sleep, or trying to take the baby away, or poke her. With my previous birth, the hospital didn’t respect my wishes. They gave my (first) daughter the Hep B shot, even though I declined it! They also gave her antibiotics and she got thrush.”
As an HBAC mom, what did you find was the most comforting part(s) of your home birth?
Cassia, “My provider knew me. The appointments were around 1 hour each. She had read my birth stories. And she was cheering me on. There were no in-betweens, no need to wait on the nurse to alert the provider and then get back to me. There was no machine acting as the monitor, with the nurse and provider attention divided. The focus was on me. Actually, my next birth ended up at a hospital where I labored mostly in triage with only one or two check-ins over several hours. My husband had to pull someone in to make sure a provider was there for the birth because they didn’t believe it would go as quickly as it did. So the difference between the two models was very stark.”

Caroline, “Having control of my own birth. My team responding to my needs as they developed. No interference or pushback. I could move around. When I wanted to do something, I just did it. I was already home, so when the baby was born, she was already home too. With her family. No strangers. Such a delicate experience to be with strangers.”

HBAC Success Stories
I’ve witnessed women labor in the safety of their homes, supported by midwives and doulas, and welcome their babies vaginally after a previous cesarean. The joy, relief, and empowerment in those moments are unmatched.
Birth is never one-size-fits-all. Whether your story unfolds entirely at home or includes a hospital transfer, your strength and determination remain the center.
Looking back, what would you change if anything? What do you wish you did differently? Are you satisfied with your HBAC outcome?
Cassia, “Change? That’s hard to say. The hardest part was that I felt like a first time mom. I’d had four previous babes, but three were inductions and one started with my water breaking and then I was given pitocin. So I had no idea what to expect with spontaneous labor and was really nervous about that. I wish I had relaxed more and called my doula earlier. I held off because I didn’t want to bother her too early. But she was a good friend who helped me recenter myself and feel calmer during labor.
And, like I said before, I’d be more mindful to rest afterward. I think it is harder for me to do that in my home, the environment where I am usually the caretaker. Hiring a postpartum doula would be a good idea for those who can afford that.
My biggest regret is actually a 4th trimester one. My midwife identified a tongue tie in my babe. I thought the pinching I was experiencing was normal, but when I mentioned it after she asked how nursing was going, she examined his latch and tongue mobility and then recommended I get it checked by an ENT. I chose to have it corrected, but I wish I hadn’t gone down that path as he did have some healing issues and the tongue tie pinching hadn’t been too bad for me. But, while I regret the way it played out, it wasn’t her fault and was actually a credit to her that she was attentive enough to pick up on it! I later learned from a dentist that most of my older children also had tongue ties. In retrospect, it’s surprising that the tongue tie wasn’t caught with my first, when I had a lot more challenges with nursing and he struggled to gain weight.
But overall my HBAC ended up my best pregnancy and birth experience. Hands down. I wish I’d been able to do it with the next births as well!”

Caroline, “I would have had my team stay home longer, and come to me later. I had them come too soon. I wish I would have hired Maegan to shoot video.”

Shoshanah, Is/are there any factors you prefer to consider?
“There are several factors that I take into consideration when taking on an HBAC client.
- Birth history – I review their previous operative reports for the type of incision, closure, & any complications during the surgery. We review their previous pregnancies, labors, and births, and look at what factors led to the final outcome. We also talk about how recovery went and if there were any complications or infections.

- Location – As with any of my clients, they need to be within my service area. Anyone in my service area is close enough to a hospital that can provide emergency services. If they are located outside of my service area, they have the option to find a place to birth within my travel radius.
- Motivation – They have to want to give birth at home and not be choosing the option because they are avoiding/afraid of the hospital. There is a distinct difference.


- Family support – Their partner/primary support person needs to be 100% on board with the choice. Nerves can be supported, but fear will permeate the birth space and is a challenge to overcome. I love when partners, kids, & other support people join us for prenatal visits.
- Education – The client needs to fully understand the risks and benefits of having an HBAC. They need to understand the process of birth, the importance of working through any emotional and/or physical trauma prior to labor (as much as possible).”

From the ICAN website, “Have you had a c-section and need support from other moms who have been there? Do you want to promote normal, evidence-based birth practices? Do you want to learn how to prevent an unnecessary c-section? Are you looking for information about how to turn breech babies and vaginal breech birth options in Atlanta? If you answered yes to any of these questions, you belong with ICAN! The cesarean rate in the United States is 32.8% Help us to reduce that number, one birth at a time.”
ICAN is active on IG, FB and has their own MB. You can read provider reviews, attend gatherings and link up with our families, for the ultimate support system!
Final Thoughts on HBAC
HBAC is not the right choice for everyone, but it can be a beautiful option for families who feel called to birth at home after a cesarean. The key is education, preparation, and a trusted care team.
If you’re considering HBAC in Atlanta, I’d love to connect. As a birth photographer and part of the Atlanta Birth Collective, I’ve supported families through both VBACs and HBACs, and I know how powerful it is to have these moments beautifully documented.
Contact me here to learn more about hiring an experienced doula and support for your HBAC journey.
HAVE QUESTIONS ABOUT HOME BIRTH, VBAC, HBAC AND/OR HIRING AN ATLANTA BIRTH PHOTOGRAPHER + DOULA? USE THE CONTACT FORM ABOVE AND CONTACT ME TODAY!






